There are six distinct types of depression, study finds
In the near future, diagnosing and treating depression might involve a quick brain scan and treatment options based on unique brain patterns

In the near future, diagnosing and treating depression might involve a quick brain scan, helping to identify the most effective treatment options based on an individual's unique brain patterns.
Researchers at Stanford Medicine, led by Dr. Leanne Williams, have made significant strides in this direction. Their groundbreaking study, soon to be published in Nature Medicine, highlights how combining brain imaging with machine learning can reveal distinct subtypes of depression. These insights could transform how treatments are matched to patients, moving away from the current trial-and-error approach.
Depression isn't a one-size-fits-all condition. Dr. Williams, the Vincent V.C. Woo Professor of Psychiatry and Behavioral Sciences and the director of Stanford Medicine’s Center for Precision Mental Health and Wellness, emphasizes the need for better methods to tailor treatments to individual patients. “The goal of our work is figuring out how we can get it right the first time,” she said. This focus stems from personal loss; Dr. Williams’s partner succumbed to depression in 2015, which has driven her dedication to the field of precision psychiatry.
Statistically, about 30% of people with depression suffer from treatment-resistant depression, meaning they don't respond to multiple therapies. Even for the rest, up to two-thirds experience only partial relief from their symptoms. This frustrating reality highlights the necessity of more precise methods to match patients with effective treatments.
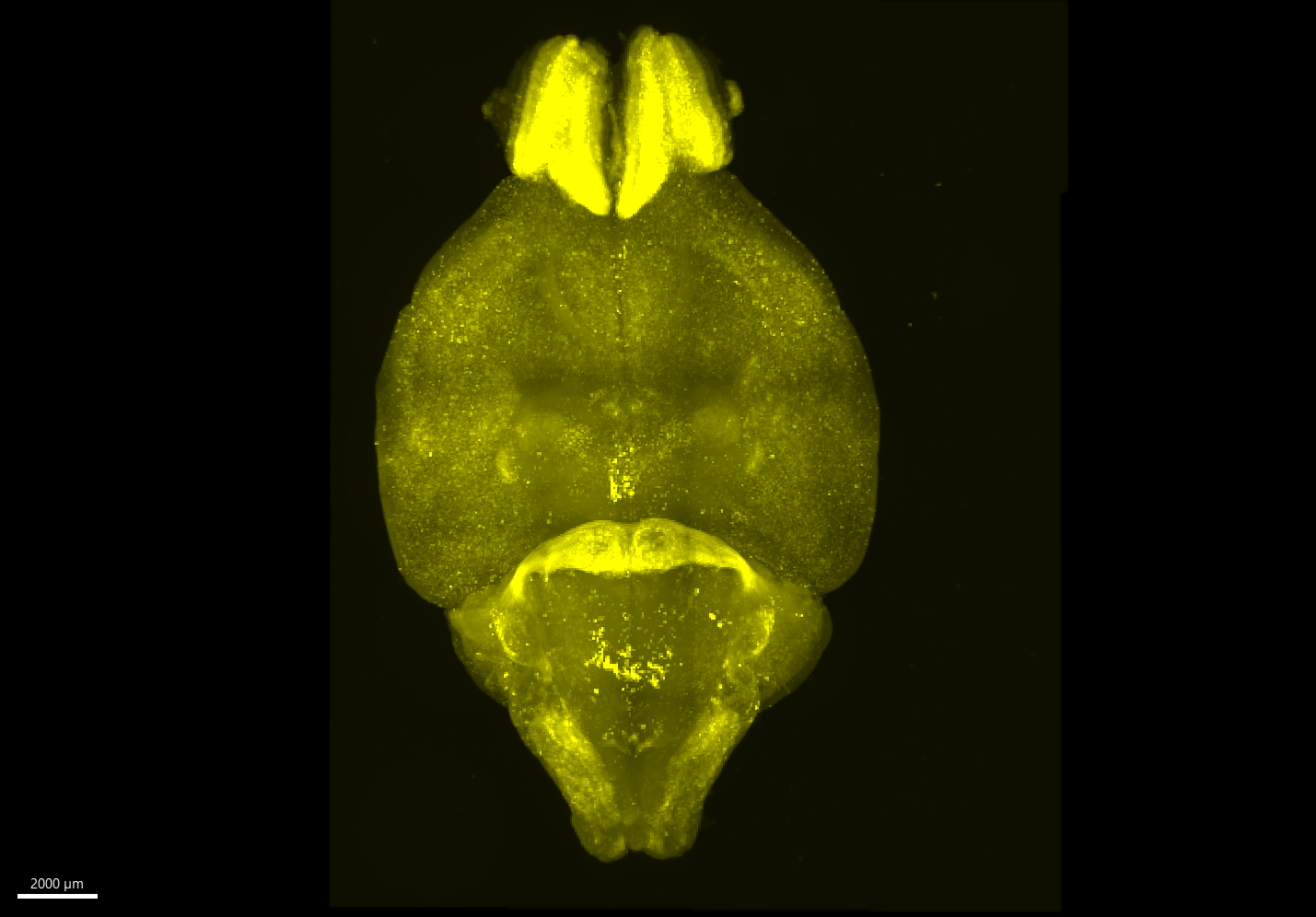
Dr. Williams's study involved 801 participants diagnosed with depression or anxiety. Using functional MRI (fMRI), a technology that measures brain activity, the researchers scanned the participants' brains both at rest and while they engaged in tasks testing their cognitive and emotional functions. They focused on specific brain regions and the connections between them, known to play a role in depression.
With the help of machine learning, particularly cluster analysis, the researchers identified six distinct patterns of brain activity among the participants. These patterns, referred to as “biotypes,” offer a new lens through which to understand and treat depression.
Related Stories
The study revealed that different biotypes responded differently to treatments. For instance, patients with overactivity in cognitive brain regions responded best to the antidepressant venlafaxine (Effexor).
Those with high activity in regions tied to depression and problem-solving showed better results with behavioral talk therapy. Conversely, individuals with lower activity in attention-related brain circuits were less likely to benefit from talk therapy.
These findings align with what scientists know about brain function and treatment mechanisms. Dr. Jun Ma from the University of Illinois Chicago, a co-author of the study, explains that the regions with high activity in certain biotypes likely make patients more receptive to learning new skills through therapy. For those with lower attention-related activity, pharmaceutical treatments might first need to address this deficit to make therapy more effective.
Dr. Williams emphasizes the novelty and significance of these findings. “To our knowledge, this is the first time we’ve been able to demonstrate that depression can be explained by different disruptions to the functioning of the brain,” she said. This approach signifies a shift towards personalized medicine in mental health, based on objective brain function measures.
Building on these insights, another study by Williams’s team demonstrated that using fMRI to identify individuals with the cognitive biotype of depression — a subtype less responsive to standard antidepressants — could predict treatment success more accurately.
They found that fMRI could predict remission likelihood in 63% of patients with this biotype, compared to just 36% without brain imaging. This improvement could greatly enhance initial treatment choices, reducing the time patients spend suffering without effective relief.
The six biotypes not only differ in brain activity but also correlate with distinct symptoms and task performance. For instance, individuals with overactive cognitive regions often experience higher levels of anhedonia, the inability to feel pleasure, and perform poorly on tasks requiring executive function. Conversely, those who respond well to talk therapy may make errors in executive functions but perform better on cognitive tasks.
Interestingly, one biotype showed no noticeable differences in brain activity compared to those without depression. This suggests that the current study may not have captured all the brain regions or mechanisms involved in depression, indicating areas for further research.
Expanding the Horizons of Depression Treatment
The research team is expanding their study to include more participants and a wider range of treatments, including medications not traditionally used for depression. They aim to refine and validate their approach, making it accessible to other clinicians.
Dr. Laura Hack, another member of the Stanford team, is already applying this imaging technique in her clinical practice. The team’s ultimate goal is to establish standardized methods that other psychiatrists can use to implement precision psychiatry in their practices.
Dr. Ma underscores the importance of this work. “To really move the field toward precision psychiatry, we need to identify treatments most likely to be effective for patients and get them on that treatment as soon as possible,” he said. This research represents a significant step towards achieving that goal, potentially transforming how depression is understood and treated.
As the field of psychiatry continues to evolve, the integration of brain imaging and machine learning promises a more personalized approach to mental health care. This could lead to quicker, more effective treatments for millions of people suffering from depression, offering hope where traditional methods have often fallen short. By uncovering the biological underpinnings of depression and tailoring treatments to individual brain patterns, the future of mental health treatment looks brighter than ever.
For more science news stories check out our New Innovations section at The Brighter Side of News.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get the Brighter Side of News' newsletter.