Researchers discover the cause of severe inflammatory bowel disease (IBD)
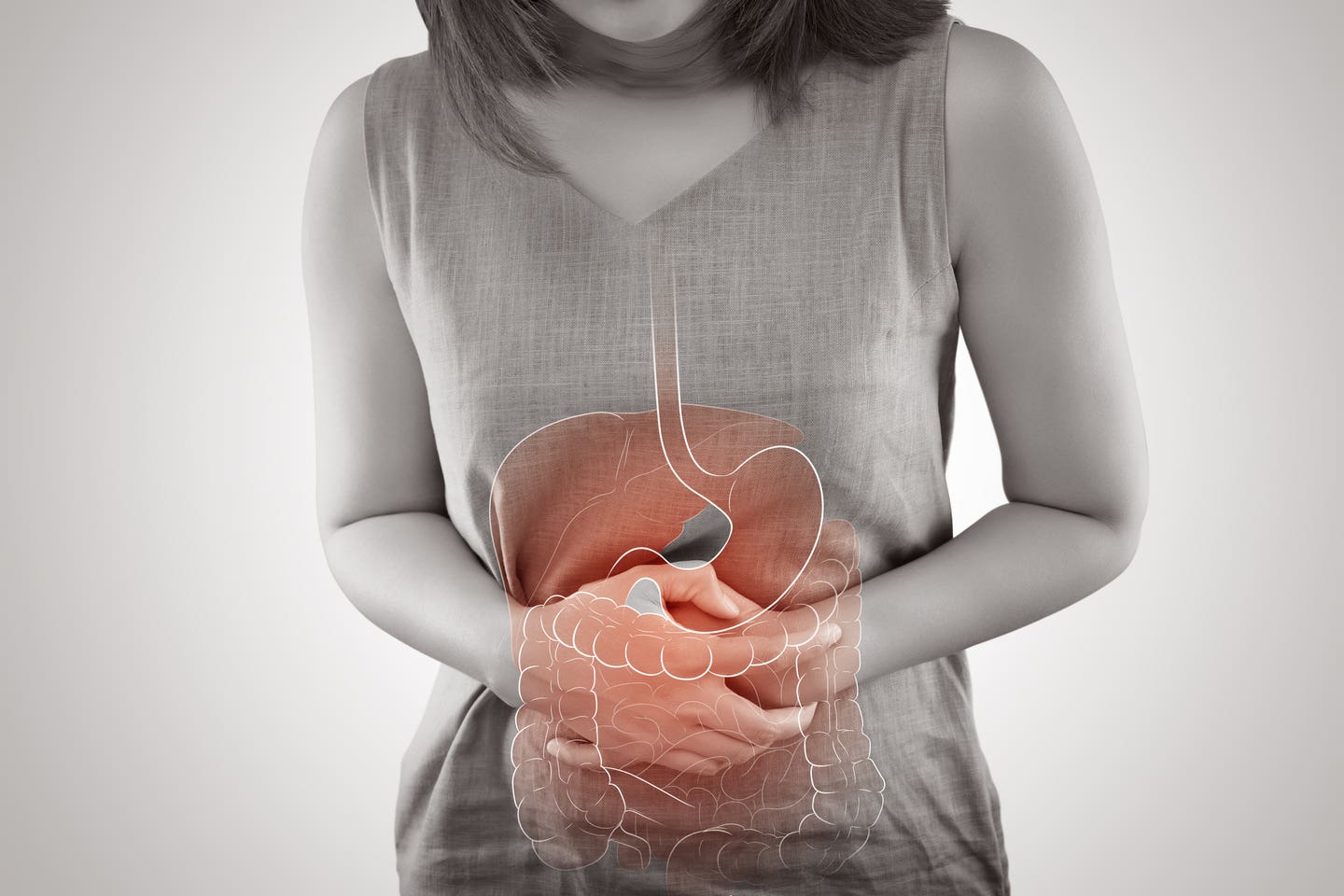
Crohn’s disease is characterized by inflammation of the lining of the digestive tract, which can cause symptoms such as abdominal pain.
[June 1, 2023: Staff Writer, The Brighter Side of News]
The smart microbe was as efficacious as a systemically delivered conventional monoclonal antibody in limiting colitis in inflammatory bowel disease. (CREDIT: Creative Commons)
Crohn's disease is a chronic inflammatory disorder that affects the digestive tract. The disease is characterized by inflammation of the lining of the digestive tract, which can cause symptoms such as abdominal pain, diarrhea, weight loss, and fatigue.
Perianal Crohn's disease is a complication of Crohn's disease that causes inflammation and ulceration of the skin around the anus, as well as other structures in the perianal area. Perianal Crohn's disease occurs in up to 40% of people with Crohn's disease and has limited treatment responses, resulting in a poor quality of life.
Cedars-Sinai investigators have identified a genetic variant that increases the risk of developing perianal Crohn’s disease, the most debilitating manifestation of Crohn’s disease.
According to the study published in the peer-reviewed journal GUT, the genetic variant generates changes to DNA that lead to a loss of protein function, which in turn, alters how the body recognizes and handles bacteria, making it less effective at fighting infections. This discovery addresses a significant area of unmet medical need, as the current therapies are not effective in treating this chronic inflammatory condition.
Related Stories:
The study, led by Dermot McGovern, MD, PhD, director of Translational Research in the Cedars-Sinai F. Widjaja Foundation Inflammatory Bowel and Immunobiology Research Institute and the Joshua L. and Lisa Z. Greer Chair in Inflammatory Bowel Disease Genetics, focused on identifying genetic variants associated with the risk of developing perianal Crohn’s disease.
The investigators analyzed genetic data from three independent cohorts of patients with Crohn’s disease, including a Cedars-Sinai cohort, an international genetics cohort recruited from over 20 countries, and a cohort recruited from seven academic research medical centers throughout the United States. The three groups totaled 4,000 patients with perianal Crohn’s disease and more than 11,000 Crohn’s disease patients without this complication.
The team of scientists compared the cohorts to see if they could detect genetic loci, which are areas of the genome associated with developing this manifestation. The team identified 10 novel genetic loci and 14 known inflammatory bowel disease loci to be associated with the development of perianal complications.
Perianal Crohn’s disease (pCD) occurs in up to 40% of patients with CD and is associated with poor quality of life, limited treatment responses and poorly understood aetiology. (CREDIT: BMJ)
During the functional characterization analysis, the team focused on a single change in a specific gene, called a SNP, that was associated with perianal Crohn’s Disease. This genetic variant affects a protein called Complement Factor B (CFB), which leads to a loss of function of this protein that is important for fighting infections, which may be why patients with this genetic change are more likely to have the condition. The investigators performed multiple analyses to confirm that there really is a loss of function in CFB, which can have a dramatic impact in the body.
“In the case where you have this mutation that leads to a nonfunctional protein, you don't get the normal signaling cascade, and the body doesn't recognize the bacteria as being harmful, and thus those bacteria are not eliminated,” said Kathrin Michelsen, PhD, a research assistant professor of Medicine and Biomedical Sciences at Cedars-Sinai and co-senior author of the study. “So, for those patients who have perianal Crohn’s disease, there are connections that form from the rectum to the skin area. And those tunnels are full of bacteria that are not being eliminated.”
Inflammatory bowel disease, or IBD, is when there is inflammation, or swelling, in the gastrointestinal (GI) tract and a lifelong immune response. (CREDIT: Creative Commons)
Michelsen also noted the study demonstrates an important role for the alternative complement pathway and CFB in the development of perianal Crohn’s disease. The findings also suggest that targeting the alternative complement pathway may be a novel therapeutic approach for treating this disabling manifestation of Crohn’s disease.
“These genetic variants often predispose to more than one condition, and we believe this discovery potentially has ramifications for other diseases as well, not just Crohn's disease,” said McGovern.
Indeed, the discovery of this genetic variant has far-reaching implications for the treatment and prevention of other inflammatory bowel diseases and autoimmune disorders.
Autoimmune diseases occur when the body’s immune system mistakenly attacks its own tissues, leading to chronic inflammation and damage. They include conditions such as rheumatoid arthritis, lupus, and multiple sclerosis, among others.
While these diseases are often viewed as distinct entities, they share many genetic and biological pathways. For example, many autoimmune diseases involve dysfunction of the immune system’s complement system, a network of proteins that helps to identify and destroy harmful pathogens.
The complement system is also involved in the development of inflammatory bowel diseases, including Crohn’s disease and ulcerative colitis. In these conditions, the complement system can become overactive, leading to chronic inflammation and tissue damage in the gut.
The discovery of the genetic variant associated with perianal Crohn’s disease suggests that dysfunction of the complement system may be a key factor in the development of other inflammatory bowel diseases and autoimmune disorders as well.
This insight could pave the way for new therapies that target the complement system to prevent or treat a range of autoimmune and inflammatory conditions.
For example, there are already drugs on the market that target components of the complement system. These drugs have shown promise in clinical trials for a range of autoimmune and inflammatory conditions, including lupus and paroxysmal nocturnal hemoglobinuria.
In addition, the discovery of the genetic variant associated with perianal Crohn’s disease could help researchers identify new drug targets for these conditions. By understanding the underlying biological mechanisms that lead to chronic inflammation and tissue damage, scientists can design drugs that target specific pathways involved in these processes.
Overall, the discovery of the genetic variant associated with perianal Crohn’s disease represents a major step forward in our understanding of autoimmune and inflammatory diseases. By identifying the genetic and biological pathways that lead to these conditions, researchers are opening up new avenues for the development of targeted therapies that could improve the lives of millions of people around the world.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get the Brighter Side of News' newsletter.
Joseph Shavit
Head Science News Writer | Communicating Innovation & Discovery
Based in Los Angeles, Joseph Shavit is an accomplished science journalist, head science news writer and co-founder at The Brighter Side of News, where he translates cutting-edge discoveries into compelling stories for a broad audience. With a strong background spanning science, business, product management, media leadership, and entrepreneurship, Joseph brings a unique perspective to science communication. His expertise allows him to uncover the intersection of technological advancements and market potential, shedding light on how groundbreaking research evolves into transformative products and industries.