Popular diabetes, weight-loss drugs could now become even more effective
Imagine a network of proteins that could make diabetes and weight-loss drugs more effective while reducing their side effects.
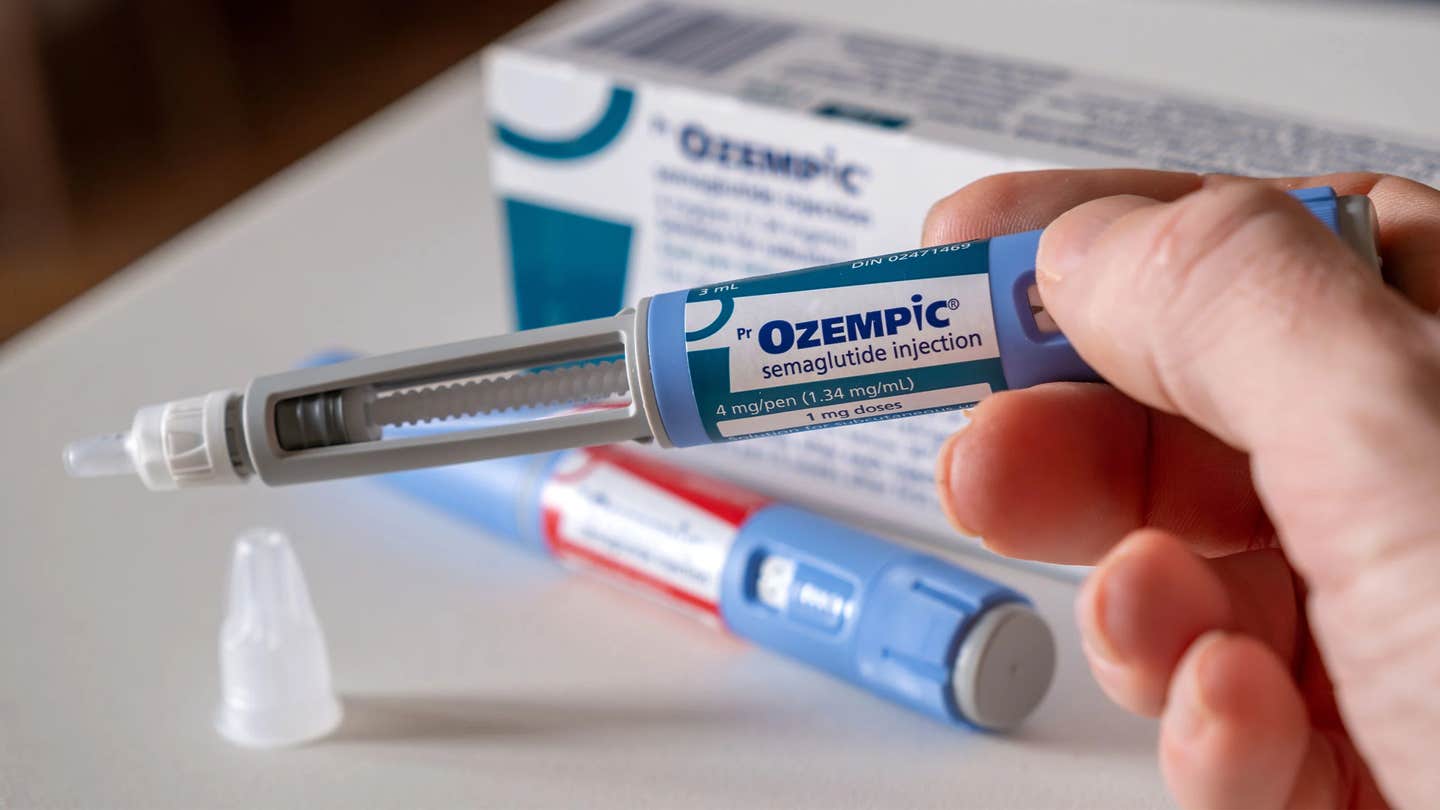
GLP-1 agonists, a class of drugs that includes semaglutides (e.g., Ozempic) and tirzepatides (e.g., Mounjaro), have recently gained attention. (CREDIT: Creative Commons)
Imagine a network of proteins in your central nervous system that could make diabetes and weight-loss drugs more effective while reducing their side effects. Researchers at the University of Michigan have discovered that two proteins, melanocortin 3 and melanocortin 4, found primarily on the surface of brain neurons, play a crucial role in regulating feeding behavior and maintaining energy balance.
This breakthrough research, published in the Journal of Clinical Investigation, opens new possibilities for enhancing popular diabetes and weight-loss medications.
These proteins impact everything from sensing long-term energy stores to processing gut signals about short-term fullness or satiety, explains U-M physiologist Roger Cone, the study's lead researcher.
GLP-1 agonists, a class of drugs that includes semaglutides (e.g., Ozempic) and tirzepatides (e.g., Mounjaro), have recently gained attention for their effectiveness in treating type 2 diabetes, obesity, heart disease, and potentially addiction. These drugs mimic a natural hormone produced by the gut when it is full, signaling the brain to reduce feeding behavior.
"So the obvious question for us was: How do these GLP-1 drugs, which work by manipulating satiety signals, function when we prime the melanocortin system?" said Cone, a professor of molecular and integrative physiology at the U-M Medical School and director of the U-M Life Sciences Institute.
In their study, Cone and his team used mouse models to test the effects of several hormones that reduce food intake. They compared results in normal mice with mice genetically lacking the MC3R protein, mice given chemicals to block MC3R activity, and mice administered a drug to increase MC4R activity. MC3R naturally decreases the activity of MC4R, so blocking MC3R and increasing MC4R activity produce similar effects.
In all cases, the team, including Naima Dahir, the study's first author and a postdoctoral research fellow in Cone's lab, found that adjusting the melanocortin system—by inhibiting MC3R or increasing MC4R activity—made the mice more sensitive to GLP-1 drugs and other hormones affecting feeding behavior. Mice given a GLP-1 drug combined with an MC4R agonist or MC3R antagonist showed up to five times more weight loss and reduced feeding than those receiving only GLP-1 drugs.
"We found that activating the central melanocortin system hypersensitizes animals to the effects of not just GLP-1s, but to every anti-feeding hormone we tested," Cone said.
Moreover, the researchers observed brain activity to understand potential side effects. They measured activity in areas thought to trigger nausea in response to GLP-1 drugs and found no increased activation when GLP-1 drugs were combined with changes to the melanocortin system. However, priming the melanocortin neurons significantly increased GLP-1 drug activation in the brain's hypothalamic feeding centers.
The findings suggest that combining existing GLP-1 drugs with an MC4R agonist could increase drug sensitivity by up to fivefold without boosting unwanted side effects. This approach could allow patients who are sensitive to side effects to take lower doses or improve results for those who have not responded to existing dosages. However, further drug development and clinical testing are needed before this can be applied to human patients.
Although the research has been conducted only in mouse models, Cone is optimistic about its relevance to humans.
"The melanocortin system is highly conserved in humans," he said. "Everything we've observed in the mouse over the past decades studying these proteins has also been found in humans, so I suspect that these results would also be translatable to patients."
By harnessing the power of the melanocortin system, there is potential to revolutionize the treatment of diabetes and obesity, making medications more effective and reducing side effects. This innovative approach offers hope for more effective therapies, potentially benefiting millions of patients worldwide.
Mechanisms of Semaglutide and Tirzepatide for Weight Loss
Semaglutide (Brand Names: Ozempic, Wegovy)
Mechanism of Action:
- GLP-1 Receptor Agonist: Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist. GLP-1 is a hormone that is naturally produced in the gut and released in response to food intake.
- Appetite Suppression: Semaglutide acts on the GLP-1 receptors in the brain, particularly in areas involved in appetite regulation, such as the hypothalamus. This action helps to reduce hunger and increase feelings of fullness, leading to a decrease in food intake.
- Slowed Gastric Emptying: By slowing down the emptying of the stomach, semaglutide helps to prolong the feeling of fullness after meals, which can help reduce overall calorie consumption.
- Insulin Secretion and Sensitivity: Semaglutide enhances insulin secretion in response to meals and improves insulin sensitivity, which helps in better blood glucose control. Although primarily beneficial for diabetes management, this also supports weight loss by stabilizing blood sugar levels and reducing cravings.
Tirzepatide (Brand Name: Mounjaro)
Mechanism of Action:
- Dual Receptor Agonist: Tirzepatide is a dual agonist, acting on both GLP-1 and glucose-dependent insulinotropic polypeptide (GIP) receptors. GIP is another incretin hormone that works alongside GLP-1 to regulate insulin secretion and appetite.
- Enhanced Appetite Regulation: By targeting both GLP-1 and GIP receptors, tirzepatide offers a more comprehensive approach to appetite suppression and satiety, leading to more significant reductions in food intake compared to agents that target GLP-1 alone.
- Improved Metabolic Profile: Tirzepatide’s dual action helps in better insulin secretion and sensitivity, as well as enhanced fat metabolism, contributing to greater weight loss and improved overall metabolic health.
- Slowed Gastric Emptying: Similar to semaglutide, tirzepatide also slows gastric emptying, which aids in prolonged satiety and reduced calorie intake.
Note: Materials provided above by the The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get the Brighter Side of News' newsletter.
Joshua Shavit
Science & Technology Writer | AI and Robotics Reporter
Joshua Shavit is a Los Angeles-based science and technology writer with a passion for exploring the breakthroughs shaping the future. As a contributor to The Brighter Side of News, he focuses on positive and transformative advancements in AI, technology, physics, engineering, robotics and space science. Joshua is currently working towards a Bachelor of Science in Business Administration at the University of California, Berkeley. He combines his academic background with a talent for storytelling, making complex scientific discoveries engaging and accessible. His work highlights the innovators behind the ideas, bringing readers closer to the people driving progress.