New treatment for early breast cancer eliminates all signs of disease
Delivering a targeted immunotoxin into breast ducts via openings in the nipple wiped out all visible and invisible precancerous lesions

[June 23, 2022: Amy Mone, Johns Hopkins Medicine]
A compound in the venom called melittin could destroy breast cancer cells within an hour. (CREDIT: Creative Commons)
Delivering a targeted immunotoxin into breast ducts via openings in the nipple wiped out all visible and invisible precancerous lesions in laboratory studies, led by researchers at the Johns Hopkins Kimmel Cancer Center, of very early stage breast cancers.
A description of the work performed on mice, which the authors say provides a strong pre-clinical foundation for conducting feasibility and safety trials with patients who have stage 0 breast cancers, is published in the Proceedings of the National Academy of Sciences.
Stage 0 breast cancer, also known as ductal carcinoma in situ (DCIS), is characterized as the presence of abnormal, precancerous cells inside milk ducts in the breast, and it affects about 69,000 women each year in the United States. Many women have breast removal surgery and radiation treatments for these very early cancers, and in some cases, they receive chemotherapy or hormone therapies, says senior study author Saraswati Sukumar, Ph.D., a Johns Hopkins professor of oncology and pathology.
“In our research, we proposed an alternative treatment in which injecting the immunotoxin drug through the duct could result in cleaning out the DCIS,” says Sukumar. “To our big surprise, the drugs killed every single lesion present in that breast duct. I had never seen such dramatic results in my life.”
Related Stories:
During their investigations, the researchers first assessed the cell-killing effects of HB21(Fv)-PE40, a targeted immunotoxin, in four cell lines of different molecular subtypes of breast cancer. The toxin consists of HB21, a monoclonal antibody — a protein that can bind to a specific target (in this case, to the human transferrin receptor, a carrier protein found in breast cancers). HB21 is fused to PE40, a fragment of a bacterial toxin that halts protein production in the cells and leads to cell death.
Results showed that the treatment induced strong cancer-killing effects in all cell lines. The researchers also administered the treatment to about 10 mice to look for toxins circulating in the blood after treatment, and found no toxins five to 30 minutes after injection.
Next, they injected HB21(Fv)-PE40 into the breast ducts of two mouse models of DCIS: MCF7 and SUM225. In MCF7 mice, the treatment was given once per week for three weeks. Treatments were followed up with noninvasive imaging. To compare, they also administered the treatment into the body and delivered the HB21 antibody alone into the ducts in some of the mice.
The two models represented all of the classifications for common types of human breast cancers: estrogen and progesterone receptor-positive and human epidermal growth factor receptor 2 (HER2) negative, estrogen and progesterone receptor-negative and HER2-positive.
In the MCF7 model, those receiving toxin treatment injections in the body had slower tumor growth. However, tumors recurred after cessation of treatment around day 26. On the other hand, in the model that received the treatment through the ducts, the tumors disappeared within two weeks of completing two of the three treatments, and no recurrence was detected via imaging even after 61 days.
On day 32, investigators conducted pathology exams of the mammary glands — two from each group. They found tumor cells were absent, and the architecture was consistent with normal mammary glands. Similar analysis of the remaining samples after 61 days showed invasive tumors in the model receiving only HB21, small tumors in those treated in the body cavity and no tumors in those receiving the toxin treatment through the ducts.
In the SUM225 model, a pilot experiment with the toxin treatment showed clearance of tumors in as early as two weeks of treatment, as seen via imaging. No recurrence was observed until the experiment was terminated at day 48. A second experiment tested the same dose and a 1/10th dose of the treatment, as well as HB21 antibody alone, in some samples.
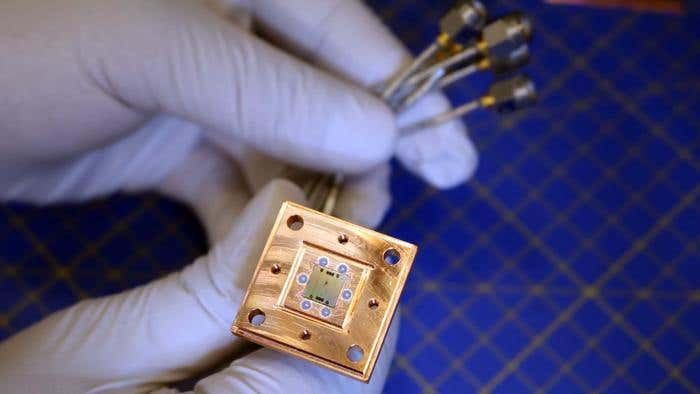
Dr. Guannan Wang performs intraductal injection under a microscope. (CREDIT: Qinxin Jiang)
The majority of the mammary glands were tumor-free after the full intraductal treatment, with weaker effects seen with the lower dose. SUM225 tumors were found to grow aggressively at the in-duct location. Pathology studies demonstrated that HB21 antibody alone had little effect, while the immunotoxin conjugate treatment showed a significant effect on tumor reduction.
The treatment was well tolerated, with no side effects from the toxin or injection.
Since most low-grade DCIS will not progress, active surveillance and hormone therapy are recommended, with larger lesions often treated more aggressively, Sukumar says. “This larger and higher-grade DCIS may be the lesions where instilling immunotoxin intraductally would be most beneficial,” she says. The big advantage is that giving the immunotoxin through the intraductal route allows it to reach all the cancer lesions in the ductal tree, eliminating even those that are not visible by imaging of the breast.
“A possible clinical study would look something like this,” Sukumar says. “A week or two before surgery, investigators may administer women a low dose of HB21(Fv)-PE40 through a single duct, and slowly use increasing doses to determine if any immunotoxin escapes the ducts into the bloodstream and affects liver function. They also would examine the ducts after breast removal to look for changes in the tissue and its effect on precancerous lesions.
Study co-authors were Guannan Wang, Alok Kumar, Preethi Korangath, Priya Pai and Kathleen Gabrielson of Johns Hopkins, Wanjun Ding of RenMin Hospital of Wuhan University, China, and Tapan Bera, Junxia Wei and Ira Pastan of the National Cancer Institute.
The work was supported by the Janine Goebel Fund and the John Fetting Fund for Breast Cancer Prevention.
Note: Materials provided above by the Johns Hopkins Medicine. Content may be edited for style and length.
Like these kind of feel good stories? Get the Brighter Side of News' newsletter.
Joseph Shavit
Head Science News Writer | Communicating Innovation & Discovery
Based in Los Angeles, Joseph Shavit is an accomplished science journalist, head science news writer and co-founder at The Brighter Side of News, where he translates cutting-edge discoveries into compelling stories for a broad audience. With a strong background spanning science, business, product management, media leadership, and entrepreneurship, Joseph brings a unique perspective to science communication. His expertise allows him to uncover the intersection of technological advancements and market potential, shedding light on how groundbreaking research evolves into transformative products and industries.