New research reveals why most long-term smokers don’t develop lung cancer
Chemicals in tobacco, such as polycyclic aromatic hydrocarbons (PAHs), damage DNA and trigger the mutations that can lead to tumors.
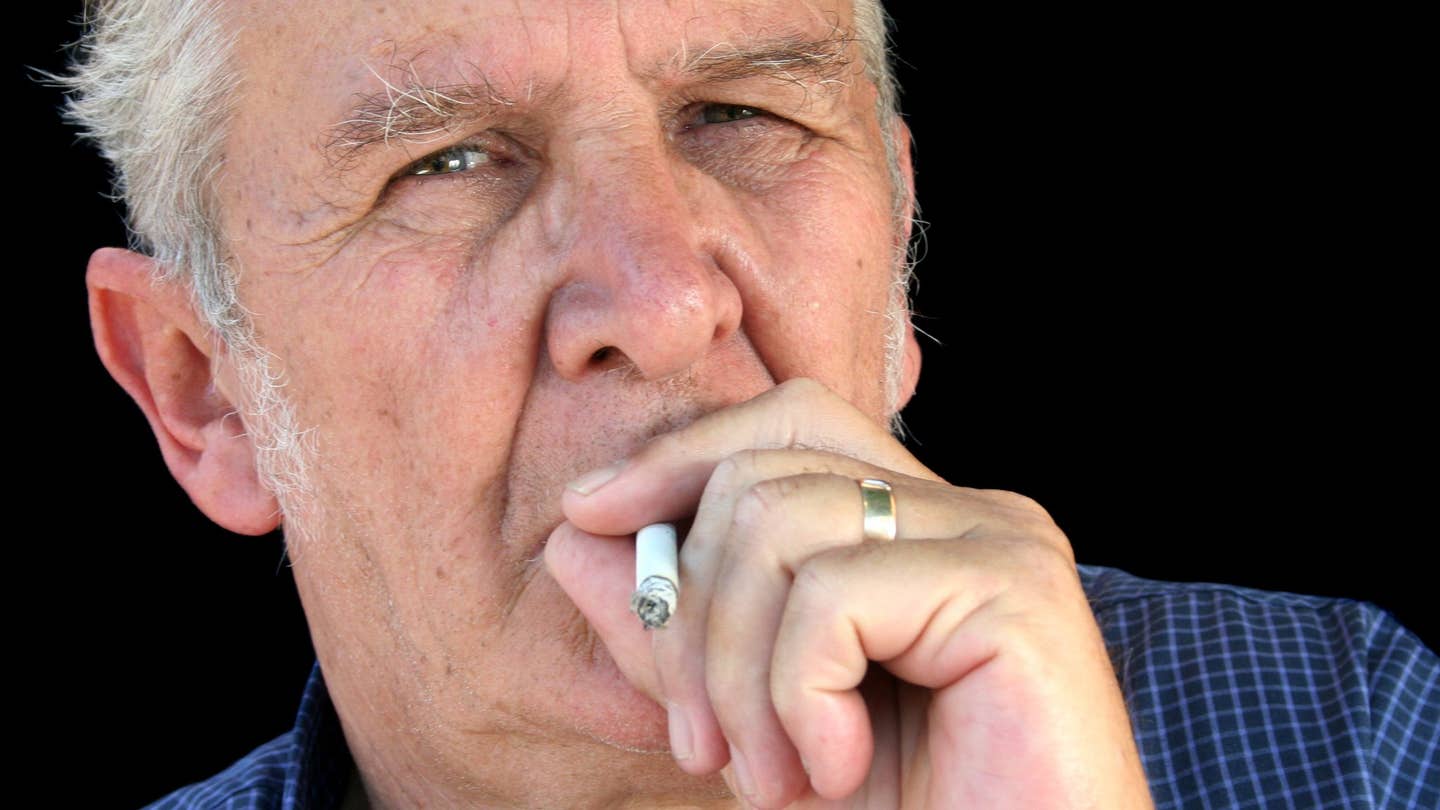
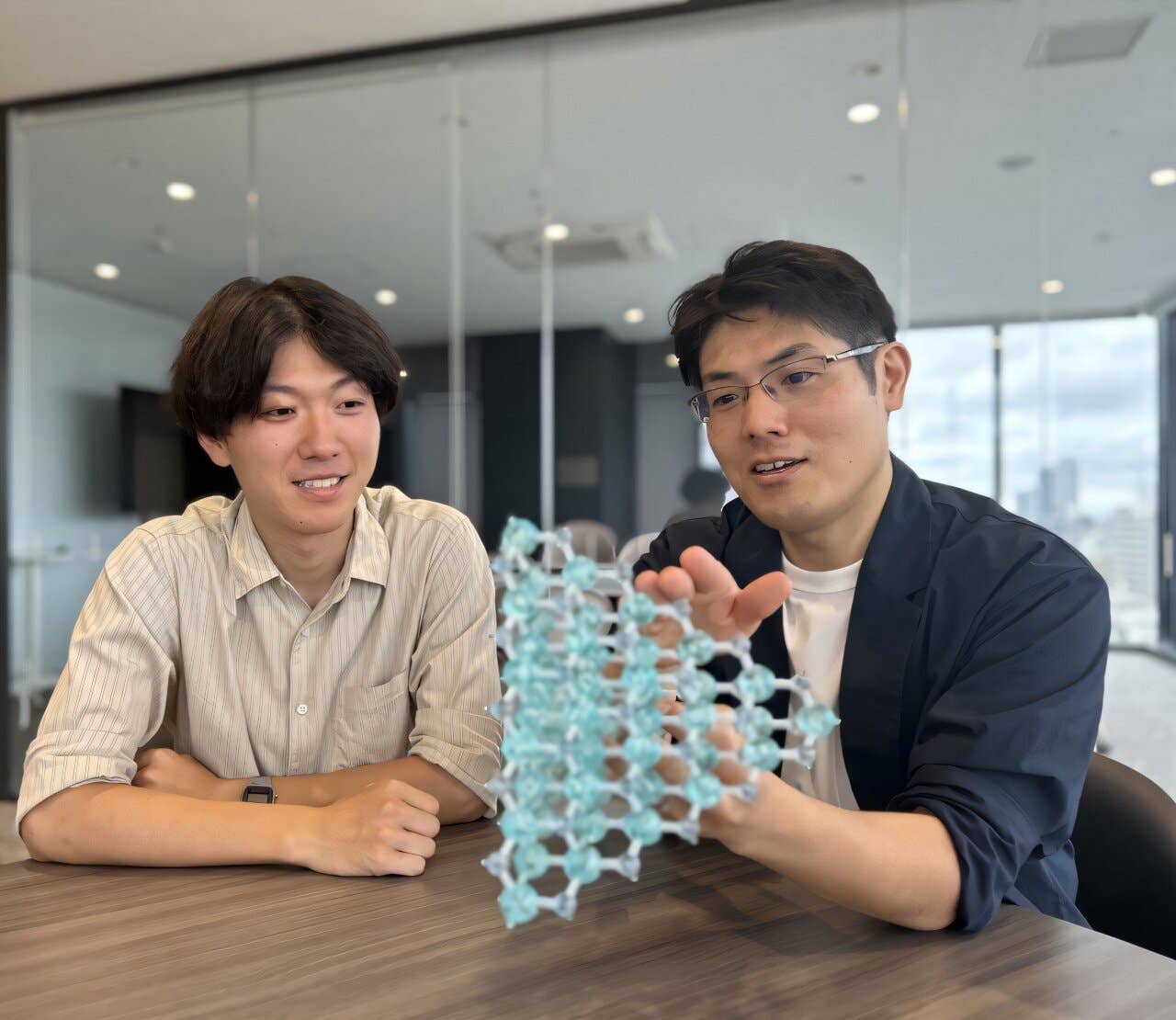
New research uncovers how smoking triggers DNA mutations in lung cells—insights that could help scientists develop better cancer prevention strategies. (CREDIT: Thinkstock)
Lung cancer remains the world’s deadliest cancer, and cigarette smoke is its chief culprit. Chemicals in tobacco, such as polycyclic aromatic hydrocarbons (PAHs), damage DNA and trigger the mutations that can lead to tumors. These toxic substances are among the most well-studied carcinogens known, making the link between smoking and lung cancer one of the most direct in medical science.
Yet, there's a surprising twist: most smokers never get lung cancer. This mystery has puzzled scientists for decades. New findings suggest that certain people may have built-in defenses that slow or limit DNA damage. “Some smokers appear to possess protective mechanisms,” researchers report, sparking fresh ideas about how cancer might be prevented or spotted early.
Understanding Risk Factors and Molecular Mechanisms
For years, studies have shown that cancer risk climbs with the number of cigarettes smoked, the length of the habit, and the age when someone quits. Still, 80 to 90 percent of smokers go their entire lives without developing lung cancer. And among those who do get sick, most are older adults. These puzzling statistics have led scientists to dig deeper, beyond habits and lifestyles, into the genetic and molecular clues that might explain why only some smokers fall ill.
Tumors from smokers often contain tens of thousands of DNA mutations, most of them somatic—acquired during life, not inherited. But scientists know far less about how mutations build up in the healthy lung cells that might eventually become cancerous. One major focus is the bronchial basal cells, located deep in the airways. These cells are considered likely precursors to squamous cell carcinoma and silently gather mutations over time.
To study these changes, scientists use a high-precision method called single-cell whole-genome sequencing (WGS). Unlike older techniques, WGS scans the entire genome of a single cell without introducing errors that come from growing cells in the lab. This allows for accurate mapping of real-time mutation patterns, even in cells that look healthy.
New breakthroughs now let researchers compare the mutation load in lung cells from smokers and non-smokers alike. By sequencing individual cells across a broad age range, scientists are learning how smoking and aging together drive cancer risk. This work is reshaping our understanding of why some lungs remain resilient despite years of smoke exposure—and why others don’t.
Related Stories
Innovations in Mutation Analysis
For decades, researchers struggled to confirm the theory that smoking causes lung cancer by inducing DNA mutations. Sequencing errors in earlier methods made it difficult to distinguish true mutations from noise, delaying progress. However, breakthroughs in single-cell genomics have overcome these limitations.
Jan Vijg, Ph.D., a leading expert in molecular genetics, developed a novel sequencing technique called single-cell multiple displacement amplification (SCMDA). This method, first described in Nature Methods in 2017, minimizes errors and improves the accuracy of mutation detection.
Researchers from the Albert Einstein College of Medicine recently used SCMDA to study lung cells from 14 non-smokers aged 11 to 86 and 19 smokers aged 44 to 81. Smokers in the study had a maximum smoking history of 116 pack-years.
The team collected bronchial epithelial cells during diagnostic bronchoscopies. These cells, among the most likely to develop into cancer, accumulate mutations from both aging and smoking. By comparing mutation rates in these groups, researchers have begun to decode the molecular footprint of smoking and its role in lung cancer risk.
Decoding Mutation Patterns
The study published in Nature Genetics, revealed that lung cells accumulate mutations as individuals age, with smokers showing significantly higher mutation rates than non-smokers. These mutations include single-nucleotide variants and small insertions or deletions. The findings reinforce the hypothesis that smoking accelerates mutation accumulation, increasing cancer risk. This aligns with broader epidemiological data showing that lung cancer is rare among non-smokers, while 10-20% of lifelong smokers develop the disease.
Interestingly, the number of mutations in smokers’ lung cells rose proportionally with pack-years of smoking but plateaued after approximately 23 pack-years. This ceiling suggests a biological limit to mutation accumulation, even in heavy smokers. According to Simon Spivack, M.D., a pulmonologist and co-senior author of the study, this plateau may reflect enhanced DNA repair mechanisms or detoxification systems in some individuals.
“The individuals who smoked the most didn’t have the highest mutation burden,” said Dr. Spivack. “This indicates that their systems may effectively counteract further DNA damage, allowing them to survive despite prolonged exposure to cigarette smoke.”
Toward Early Detection and Prevention
These findings open the door to new approaches in lung cancer research. Identifying the molecular mechanisms that protect certain smokers could lead to targeted interventions for those at higher risk.
Dr. Vijg emphasized the importance of developing assays to measure an individual’s capacity for DNA repair or detoxification. Such tools could revolutionize risk assessment and early detection strategies.
Dr. Spivack highlighted the broader implications of this research: “This may prove to be an important step toward the prevention and early detection of lung cancer risk and away from the current herculean efforts needed to battle late-stage disease, where the majority of health expenditures and misery occur.”
By combining advanced genomic techniques with epidemiological insights, researchers hope to move closer to personalized cancer prevention. This approach could help identify at-risk individuals before symptoms arise, improving outcomes and reducing the burden of late-stage disease.
The Path Forward
The research underscores the importance of bridging molecular biology and clinical practice. While smoking cessation remains the most effective way to reduce lung cancer risk, understanding the genetic and molecular basis of cancer resilience offers new hope. The ability to pinpoint individuals who are more vulnerable to the harmful effects of smoking could enable earlier interventions and better allocation of healthcare resources.
As scientists continue to refine single-cell sequencing techniques, the potential for breakthroughs in cancer prevention and treatment grows. This research not only advances our understanding of lung cancer but also sets the stage for innovations in precision medicine. By unraveling the complex interplay of age, smoking, and genetic resilience, researchers are paving the way for a future where lung cancer is not only treatable but preventable.
How does smoking affect your body?
According to the Cleveland Clinic, tobacco use harms every organ in your body. Smoking tobacco introduces not only nicotine but also more than 5,000 chemicals, including numerous carcinogens (cancer-causing chemicals), into your lungs, blood and organs.
The damage caused by smoking can shorten your lifespan significantly. In fact, smoking is the number one cause of preventable death in the United States.
Pregnant women who smoke put their unborn babies at risk, too. Possible effects on pregnancy include:
- Ectopic pregnancy, a life-threatening condition when the embryo implants outside the uterus.
- Miscarriages.
- Stillbirths.
- Birth defects, such as cleft palate.
- Low birth weight.
What other conditions may be caused or worsened by tobacco?
In addition to its known cancer risks, the Cleveland Clinic states that smoking causes many other chronic (long-term) health problems that need ongoing care. Specific smoking-related problems that need treatment include:
- Decreased HDL (good) cholesterol and increased blood pressure (increasing risks for heart attack and stroke).
- Erectile dysfunction.
- Lower oxygen to the heart and other tissues in the body (increasing risks for coronary artery disease, peripheral artery disease, and diabetes).
- More frequent routine illnesses like colds, especially in children living with smokers.
- Poorer lung function (ability to get enough oxygen) leading to COPD, asthma, bronchitis, or emphysema.
The study is titled, “Single-cell analysis of somatic mutations in human bronchial epithelial cells in relation to aging and smoking.”
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.