New proton beam therapy precisely targets and destroys cancer cells
Novel glioblastoma therapy combines precision radiation and advanced imaging, offering hope and improved survival for older patients.
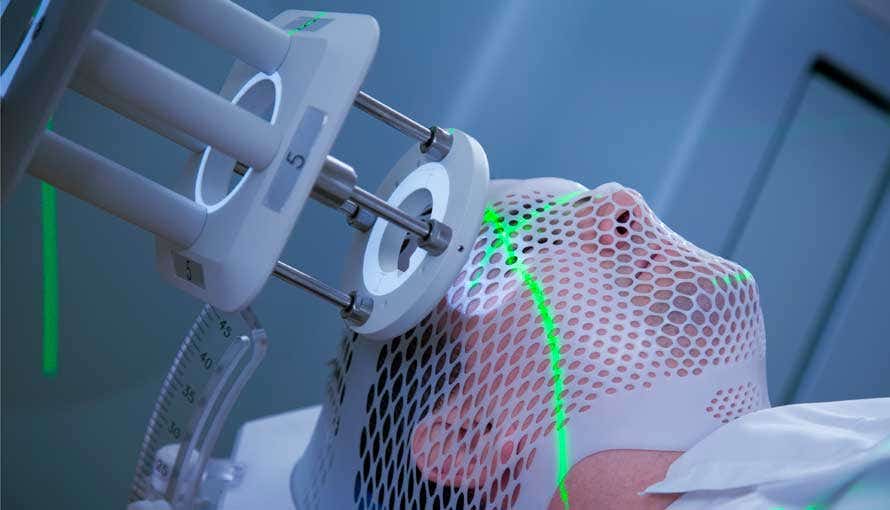
Proton beam therapy delivers targeted radiation with unparalleled precision. (CREDIT: CC BY-SA 4.0)
Glioblastoma, the most common and lethal form of primary brain cancer, presents daunting challenges. Each year, around 14,500 people in the United States face this aggressive disease. Its invasive nature makes surgical removal delicate, as tumors intertwine with healthy brain tissue.
Traditional treatments, while effective to an extent, often carry significant side effects. Published in the journal, The Lancet: Oncology, a groundbreaking approach by Mayo Clinic researchers offers a glimmer of hope, especially for older patients.
The Mayo Clinic study introduced a novel therapy combining advanced imaging techniques with proton beam radiation. Proton beam therapy delivers targeted radiation with unparalleled precision, reducing collateral damage to healthy brain tissue. This precision is crucial for glioblastoma patients, as sparing healthy tissue can significantly improve quality of life.
Advanced imaging tools, such as 18F-DOPA PET and contrast-enhanced MRI, mapped the most metabolically active areas of the tumor. "Combining advanced imaging allowed us to determine the most aggressive regions of the glioblastoma," explained Dr. Sujay Vora, the radiation oncologist leading the study. This approach ensured that radiation targeted the cancer while minimizing exposure to surrounding healthy areas.
The treatment protocol involved a short course of hypofractionated proton beam therapy. Patients received radiation over one to two weeks, a significant reduction from the traditional three to six weeks.
Concurrently, they were administered temozolomide, a chemotherapy drug known for its effectiveness against glioblastoma. Post-radiation, patients underwent six cycles of adjuvant temozolomide treatment.
The phase 2 trial included patients aged 65 and older from Mayo Clinic campuses in Arizona and Minnesota. Results were encouraging: 56% of participants were alive after 12 months, with a median overall survival of 13.1 months. Patients with favorable tumor genetics experienced even better outcomes, with survival extending to 22 months.
Dr. Vora expressed optimism, stating, "As compared to prior studies in older populations with median survival of six to nine months, these results are promising."
Related Stories
One participant, Richard Casper, credited the therapy for giving him nearly two extra years beyond his initial prognosis. Despite his eventual passing in 2023, his family cherishes the memories made during this time. "We will forever be grateful for the extra time we had with our father," said his daughter, Susan Casper.
Another participant, Nadya El-Afandi, was diagnosed in 2022. Now 15 months post-treatment, she shows no signs of tumor recurrence. El-Afandi, a mother of four, resumed her active lifestyle and recently enjoyed a snorkeling and hiking trip to Hawaii. "There's no cure yet, but this treatment has given me a quality of life that is just outstanding," she said.
Traditional radiation therapies, while effective, often expose healthy brain tissue to harmful radiation, leading to unintended side effects. By contrast, proton beam therapy minimizes these risks, making it particularly beneficial for older patients. This advancement aligns with the study’s dual goals: extending survival and preserving quality of life.
Older glioblastoma patients historically face grim prognoses, with median survival ranging from six to nine months. The use of proton beam therapy—a technology that selectively targets tumors while sparing healthy brain tissue—represents a significant step forward. This approach also reduces the burden of lengthy treatments, an important factor for older patients.
The Mayo Clinic’s work underscores the potential of integrating advanced imaging with precision therapies. "The advanced imaging along with the proton beam therapy allowed us to be more focused with radiation and protect surrounding healthy brain tissue," Dr. Vora noted. Patients not only tolerated the treatment well but also experienced improved survival outcomes.
Building on these promising results, Mayo Clinic launched a larger, randomized clinical trial known as SAGA. This study incorporates additional imaging advancements to further refine tumor visualization and treatment.
"We are now adding another component that builds upon Dr. Vora's work to help us best visualize the tumor," said Dr. William Breen, a radiation oncologist and principal investigator.
Dr. Breen emphasized that it is too early to draw definitive conclusions about the therapy’s safety and efficacy. However, the trial’s ultimate goal is clear: to transform glioblastoma treatment by making it more efficient and less burdensome for patients and their families.
El-Afandi, one of the study’s success stories, embodies the hope this research offers. Her words reflect the resilience and gratitude shared by many participants: "Every day is the best day, and I'm going to enjoy every minute of it."
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Joshua Shavit
Science & Technology Writer | AI and Robotics Reporter
Joshua Shavit is a Los Angeles-based science and technology writer with a passion for exploring the breakthroughs shaping the future. As a contributor to The Brighter Side of News, he focuses on positive and transformative advancements in AI, technology, physics, engineering, robotics and space science. Joshua is currently working towards a Bachelor of Science in Business Administration at the University of California, Berkeley. He combines his academic background with a talent for storytelling, making complex scientific discoveries engaging and accessible. His work highlights the innovators behind the ideas, bringing readers closer to the people driving progress.



