New discovery revolutionizes blood cancer treatment
Researchers develop a computational model to combat drug resistance in chronic myeloid leukemia, offering personalized treatment strategies for patients.
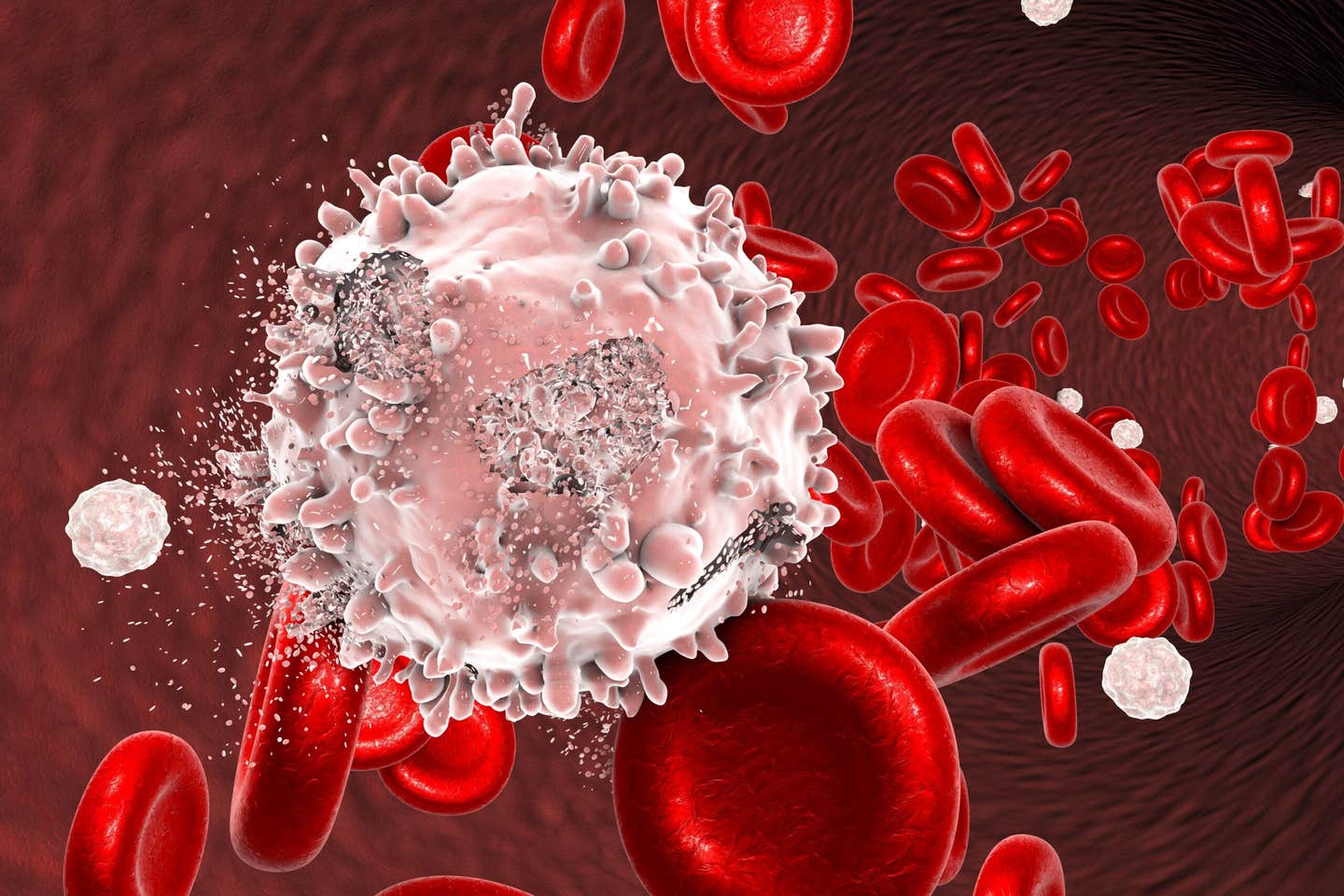
Resistance to CML therapies complicates treatment, but new computational models promise to improve outcomes with precision medicine tailored to patients. (CREDIT: CC BY-SA 4.0)
Millions of individuals rely on effective medications to manage diseases like cancer and diabetes. For those with chronic myeloid leukemia (CML), advancements in treatment selection could significantly improve outcomes. CML is a blood cancer linked to a genetic mutation known as the Philadelphia chromosome. This mutation drives uncontrolled cell growth by creating a hyperactive enzyme, Abl1 kinase. While treatments exist, resistance to these therapies remains a significant challenge.
CML is primarily treated with Abl1 inhibitors—drugs targeting the malfunctioning enzyme. The first-line treatment, imatinib, often yields positive results but falls short for approximately 25% of patients within two years. Resistance arises due to mutations in the Abl1 enzyme, altering its structure and reducing the efficacy of the inhibitors. Mutations not only impact drug binding but also influence enzymatic activity, making resistance mechanisms complex.
These mutations can make treatment decisions even more challenging. Selecting the appropriate drug to combat resistance requires precise knowledge of how each mutation impacts the enzyme's behavior. This process often involves trial and error, which prolongs patient suffering and increases treatment costs.
Furthermore, resistance mechanisms are not always straightforward. They involve intricate interactions between drug molecules and enzymes, making it difficult to predict outcomes based on traditional measurements alone.
Current approaches to combat resistance rely on measuring IC50 values, which indicate the concentration of a drug required to inhibit enzyme activity by 50%. However, IC50 values vary between assays and are influenced by numerous factors, leading to inconsistencies.
For example, data collected from different laboratories often show significant variability, reducing reliability. While useful, this method alone does not fully account for the interplay between enzyme activity, drug concentration, and mutation-driven resistance.
Recognizing the limitations of IC50-based methods, researchers have developed computational models to refine treatment selection. These models evaluate the Abl1 enzyme's catalytic activity and inhibitor interactions to determine the most effective drugs for specific mutations. The approach emphasizes a parameter termed "inhibitory reduction prowess," which better predicts resistance than traditional methods.
“We have developed a computer model that can help us identify which drugs work best for each individual patient,” explains Professor Ran Friedman from Linnaeus University. This model considers factors beyond IC50 values, such as drug concentration and enzymatic activity, providing a more comprehensive understanding of resistance.
By focusing on how mutations influence both the binding of drugs and the enzyme’s catalytic activity, the model helps pinpoint the optimal treatment strategy. This method is particularly valuable for patients who develop resistance after initial treatment, as it can identify alternative therapies that are more likely to succeed. Moreover, the model’s predictive power reduces the need for trial-and-error approaches, saving time and resources.
Drug resistance is not unique to CML; it complicates treatments for various cancers and infectious diseases. When resistant cell populations dominate, the efficacy of initial therapies declines, necessitating alternative treatments. Switching medications becomes critical, but selecting the right drug remains a complex process.
Related Stories
Jennifer Sheehan, a PhD fellow at the Norwegian University of Science and Technology (NTNU), emphasizes the importance of tailored treatments. “The new method can help those affected by chronic myelogenous leukemia,” she says.
Sheehan’s team, in collaboration with Linnaeus University and the Universidade de São Paulo, has published findings in PLOS Computational Biology highlighting the potential of computational modeling to revolutionize drug selection.
These advancements also shed light on broader challenges in treating drug-resistant diseases. Resistance mechanisms often involve complex genetic and biochemical changes that render standard therapies ineffective. Understanding these changes is crucial for developing new treatments that can outpace the evolution of resistance.
In the case of CML, insights gained from computational models could inform similar approaches for other cancers, expanding their impact beyond this specific disease.
CML treatments aim to achieve deep molecular responses—a state where the disease is virtually undetectable. Achieving this requires prolonged periods of effective therapy, often spanning over two years. However, resistance complicates long-term outcomes. The toxicity and financial burden of extended treatment further underscore the need for precision medicine.
Abl1 inhibitors target the overactive enzyme to reduce cell proliferation and suppress symptoms. Yet, different mutations respond variably to these drugs, and resistance mechanisms remain incompletely understood. For example, variations in the enzyme’s catalytic rate constant (“kcat”) suggest that mutations influence more than just drug binding.
Traditional drug selection methods compare the IC50 values of wild-type and mutated enzymes to determine relative efficacy. While a lower IC50 indicates higher potency, it does not always correlate with clinical success. Researchers argue that focusing solely on IC50 values overlooks crucial factors like enzyme stability and drug concentration dynamics.
Computational models, on the other hand, integrate these factors to provide a more accurate assessment of treatment options. By simulating how different drugs interact with specific mutations, these models offer a clearer picture of which therapies are likely to succeed. This approach not only improves patient outcomes but also reduces the risk of unnecessary side effects from ineffective treatments.
Computational models offer a promising alternative to conventional methods. By incorporating data on catalysis, inhibition, and pharmacokinetics, these models identify the best treatment options for specific mutations. This approach aligns with the broader goal of precision medicine—matching therapies to individual patient profiles for optimal outcomes.
“CML is a form of cancer that many people live with for a long time without knowing it,” notes Professor Astrid S. de Wijn of NTNU. Symptoms often remain hidden for years, making timely and effective treatment crucial once diagnosed.
While stem cell transplantation remains the most definitive cure, many patients manage their condition with tyrosine kinase inhibitors. However, the choice of medication is critical, given the presence of multiple available drugs and the need to counteract resistance.
Researchers believe that refining drug selection protocols can improve survival rates and reduce the burden of prolonged treatment. The proposed computational model not only guides treatment decisions but also advances understanding of resistance mechanisms. This innovation holds the potential to improve patient outcomes significantly while minimizing the risk of long-term treatment complications.
In a world where resistance challenges treatments for cancer and infectious diseases alike, tools like these mark a significant step forward. They exemplify how science and technology can converge to address complex medical challenges and pave the way for more effective and personalized care.
Efforts to refine these models are ongoing, with researchers exploring ways to incorporate even more data, such as patient-specific genetic information and real-time drug efficacy measurements. These enhancements could further enhance the precision of treatment recommendations, bringing the goal of personalized medicine closer to reality.
By integrating advanced computational tools with clinical insights, the medical community is taking a significant step toward overcoming one of the most persistent challenges in modern healthcare.
As these models continue to evolve, they promise to transform the landscape of cancer treatment, offering new hope to patients worldwide.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Joshua Shavit
Science & Technology Writer | AI and Robotics Reporter
Joshua Shavit is a Los Angeles-based science and technology writer with a passion for exploring the breakthroughs shaping the future. As a contributor to The Brighter Side of News, he focuses on positive and transformative advancements in AI, technology, physics, engineering, robotics and space science. Joshua is currently working towards a Bachelor of Science in Business Administration at the University of California, Berkeley. He combines his academic background with a talent for storytelling, making complex scientific discoveries engaging and accessible. His work highlights the innovators behind the ideas, bringing readers closer to the people driving progress.