New blood test promises safer, more effective cancer treatments
A groundbreaking test tailors nanomedicine treatments for leukemia patients, improving efficacy and reducing side effects through personalized therapy.
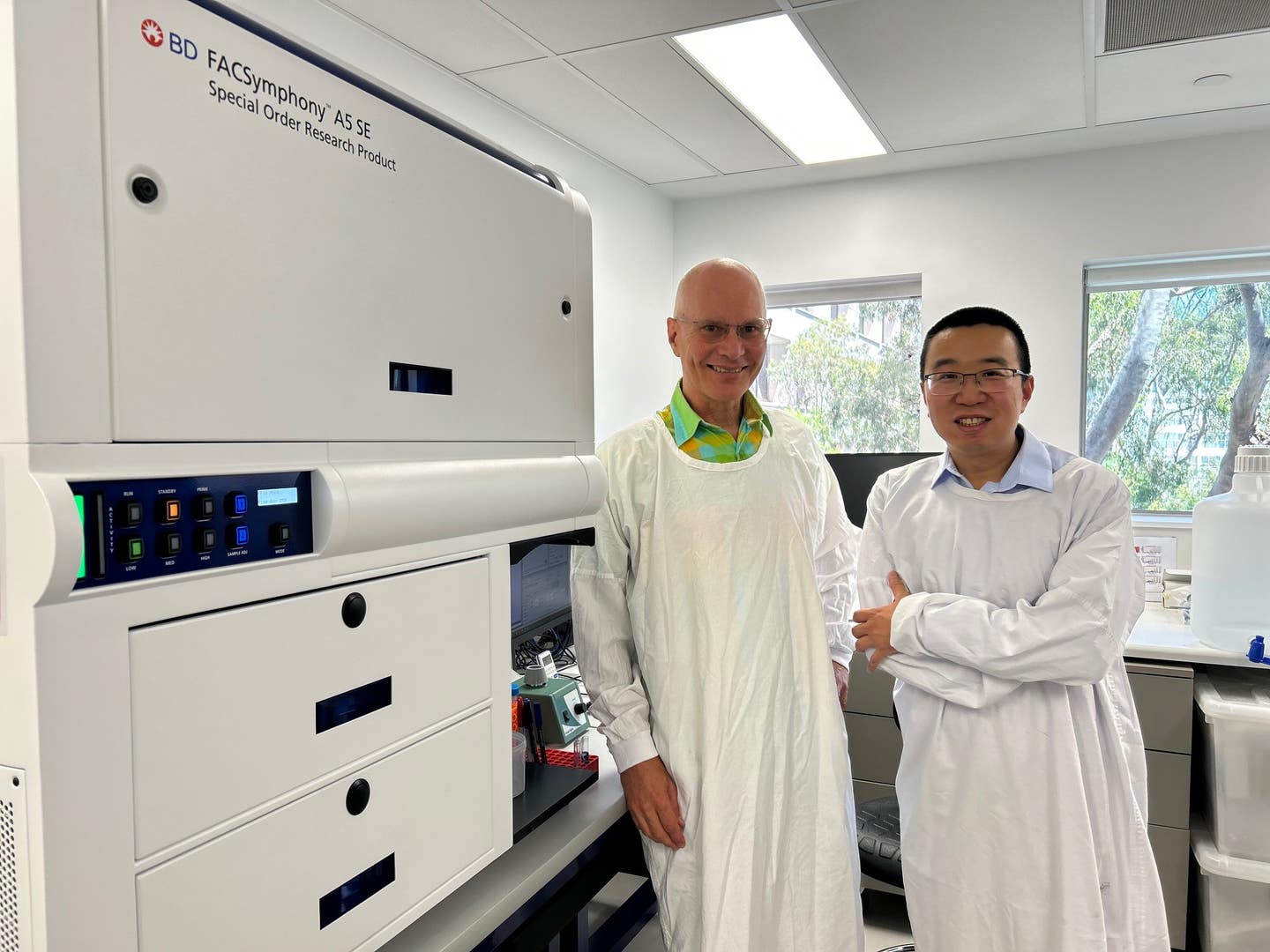
Professor Stephen Kent (left) with Dr Yi (David) Ju next to the flow cytometer in a Doherty Institute lab where they analysed blood samples. (CREDIT: Thakshila Amarasena, Doherty Institute)
A groundbreaking innovation in cancer treatment is emerging, offering a glimpse into a future of safer, more effective therapies.
Researchers have developed a test that could personalize nanomedicine-based treatments for leukemia patients, potentially improving outcomes while reducing harmful side effects. This advancement highlights the power of tailoring therapies to individual immune responses, a critical step forward in cancer care.
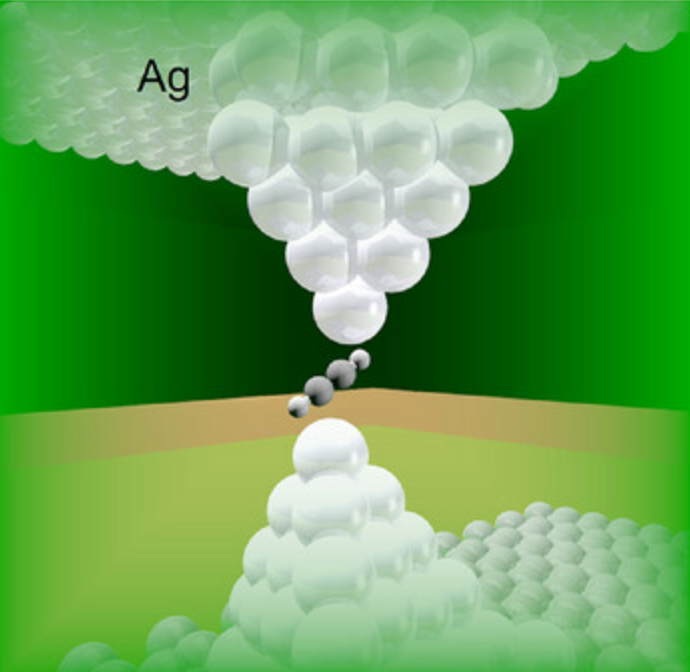
Nanomedicines are ultra-small particles engineered to deliver drugs directly to diseased cells, such as cancerous ones, while sparing healthy tissues. Despite their promise, clinical responses to these therapies vary widely among patients. Scientists at RMIT University and the Doherty Institute conducted a pioneering study to address this challenge, shedding light on why some patients benefit more than others.
The team’s innovative blood test, described in the journal ACS Nano, is the first of its kind. It assesses how different polyethylene glycol (PEG)-based nanomedicines interact with blood cells in leukemia patients. By using just a drop of blood, the test evaluates both the efficacy of these therapies in targeting cancer cells and their potential toxicity to healthy cells. The findings represent a significant step toward personalized cancer treatments.
Dr. Yi (David) Ju, who led the study, explained the potential impact: “Our study sheds light on why some cancer patients respond better to nanomedicine therapies than others. By understanding these differences, we can develop more personalized and effective treatments for leukemia patients.”
The research involved testing three PEG-based nanomedicine formulations on blood samples from 15 leukemia patients. These samples were incubated at body temperature for one hour to simulate in-body conditions. The goal was to determine which therapies were most effective at targeting cancer cells while minimizing damage to healthy immune cells.
The study revealed striking variability in patient responses. For instance, one type of PEG nanoparticle showed up to a 234-fold difference in cancer-targeting efficiency among patients.
This variability was linked to the presence of anti-PEG antibodies in the blood, which can neutralize the therapeutic effects of nanomedicines. Patients with high levels of these antibodies not only experienced reduced efficacy but also faced higher toxicity, as healthy immune cells were targeted instead of cancer cells.
Related Stories
“The greater the presence of anti-PEG antibodies in people’s blood, the less effective these therapies were at killing cancer cells. In fact, these therapies were more toxic to healthy cells,” Ju noted.
One of the tested nanomedicines, Doxil, is widely used to treat cancers like ovarian cancer, Kaposi’s sarcoma, and multiple myeloma. While not typically used for leukemia, Doxil’s performance in the study underscored the impact of individual immune profiles. For some patients, Doxil remained the most effective option, but for others, the toxicity to healthy immune cells outweighed its benefits.
The team’s own formulation of pure PEG nanoparticles emerged as the most effective targeted therapy against leukemia cells. This highlights the potential for developing next-generation nanomedicines tailored to individual patients.
The findings build on earlier research suggesting that anti-PEG antibodies—which can develop in response to mRNA vaccines—may reduce the efficacy of PEG-based therapies. This has implications for future treatments that rely on similar compounds.
Understanding the interplay between nanomedicines and individual immune systems is critical. When introduced into the bloodstream, nanoparticles interact with proteins, immune cells, and other blood components. These interactions are highly person-specific, influenced by factors such as age, genetics, lifestyle, and underlying health conditions.
Previous studies have shown that plasma from cancer patients differs from that of healthy individuals, affecting how nanoparticles behave. This variability has been leveraged for biomarker discovery and immunomodulation. However, until now, the effects of these differences on nanoparticle-based therapies had not been thoroughly investigated.
Dr. Ju and his colleagues’ innovative approach involves using a whole-blood model to simulate real-life conditions. Unlike traditional in vitro studies using cell lines or animal models, this method incorporates the complexity of human blood. By including cancer cells from leukemia patients, the researchers created an ex vivo system that closely mimics how nanoparticles interact with the immune system during treatment.
Professor Stephen Kent, a co-author from the Doherty Institute, emphasized the broader implications of the study: “Understanding individual variations in immune response could lead to more effective and safer treatments by tailoring nanoparticle formulations to each patient’s unique immune profile.”
This personalized approach could extend beyond leukemia to solid tumors, including breast and ovarian cancers. Simple blood tests may one day guide the selection of the most suitable nanomedicines for each patient, improving outcomes and minimizing side effects.
Professor Constantine Tam, another co-author, echoed the study’s significance: “Our findings indicate that we can use this knowledge to develop personalized therapies not just for leukemia but for a range of cancers.”
The researchers envision partnerships with pharmaceutical companies to refine and commercialize their technology. Such collaborations could accelerate the translation of these findings into clinical practice, bringing personalized cancer treatments closer to reality.
Despite its promise, the test is not yet available in clinical settings. With industry and government support, the team hopes to make it widely accessible in the coming years. Their innovation underscores the need for continued investment in personalized medicine to address the complexities of cancer treatment.
As the fight against cancer progresses, this research marks a pivotal moment. By unraveling the intricacies of nanomedicine interactions with individual immune systems, scientists are paving the way for therapies that are both more effective and less harmful.
The future of cancer treatment is increasingly focused on the individual, and this breakthrough is a testament to the power of personalized medicine.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.