Magnetic pulses aimed at the brain could treat insomnia, study finds
Military personnel may soon find relief from insomnia with a new brain stimulation technique designed to enhance sleep without drugs.

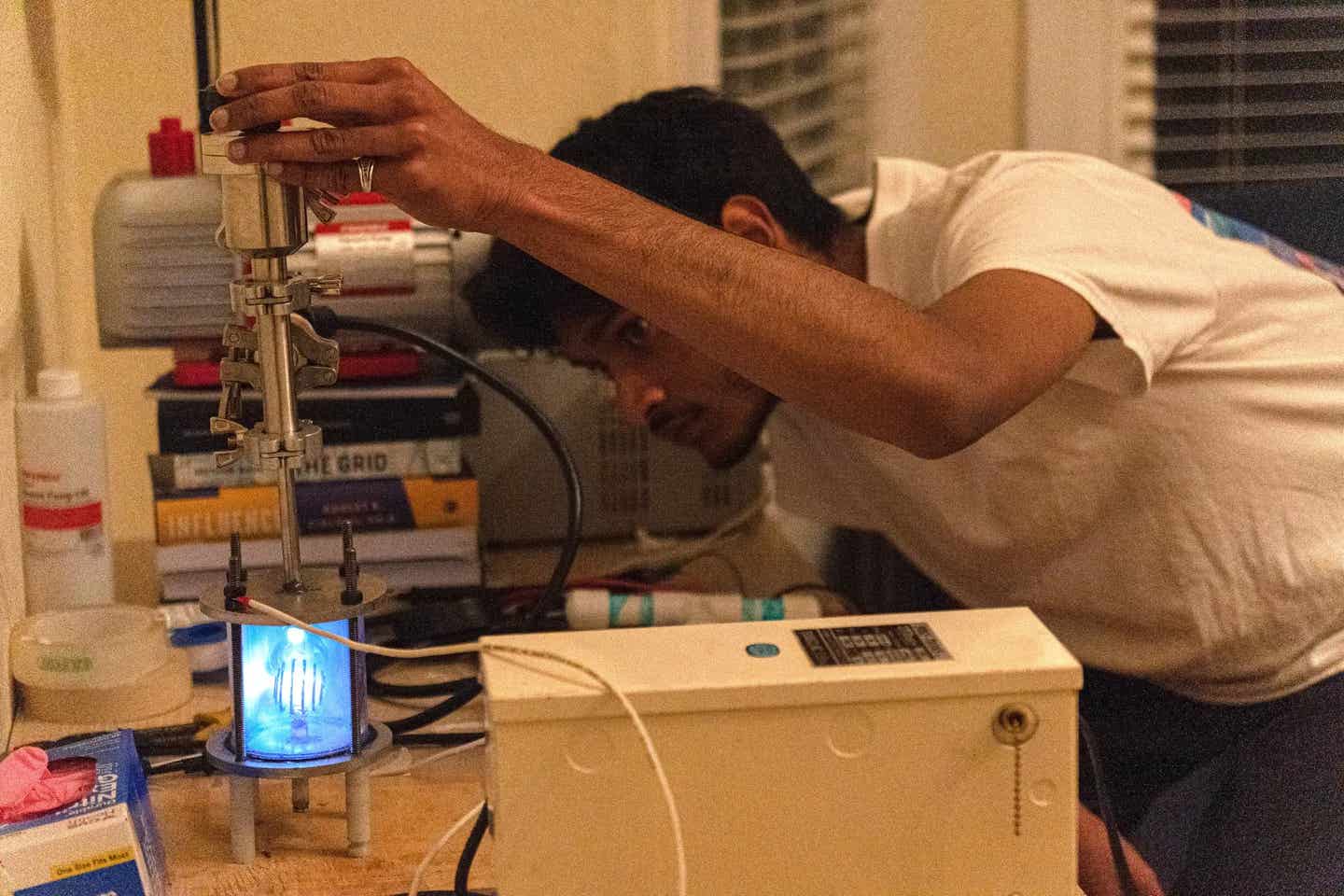
University of Arizona researchers aim to tackle military insomnia with a promising brain stimulation treatment, helping to improve sleep without medication. (CREDIT: CC BY-SA 4.0)
Military personnel frequently face sleep problems that significantly impact their readiness. With about 85% meeting criteria for sleep disorders and 25% reporting insomnia as a primary issue, the need for effective, non-drug solutions has never been more urgent.
The University of Arizona College of Medicine – Tucson aims to address this need, thanks to a $3 million grant from the Department of Defense's Congressionally Directed Medical Research Program.
Dr. William “Scott” Killgore, an Army veteran and professor of psychiatry, has spent over a decade exploring mental health factors affecting military personnel. Leading a team in the Social, Cognitive, and Affective Neuroscience (SCAN) Lab, Killgore focuses on insomnia, a common affliction that he believes is partly driven by the brain’s excessive arousal.
“Insomnia is generally believed to be caused by excessive arousal of the brain and body, often due to worry and negative thoughts before sleep,” Killgore explains. This sleeplessness results from heightened activity in the brain's default mode network (DMN), a system that processes internal thoughts and emotions, particularly during restful, introspective periods.
Killgore's team recently conducted a preliminary study targeting the DMN with transcranial magnetic stimulation (TMS). Using a handheld device, they delivered 40-second bursts of continuous theta burst stimulation, a process of sending rapid, repetitive magnetic pulses to specific brain regions.
“Many people with insomnia describe being unable to ‘turn off’ their thoughts when trying to fall asleep,” Killgore notes. The study found that by disrupting the DMN through brief stimulation, participants could achieve better sleep.
This initial research yielded promising results, showing sleep improvements after just one session of continuous theta burst stimulation. This approach is not new to mental health treatments, but targeting the DMN for insomnia is a novel application. Buoyed by these findings, Killgore’s team will now undertake an expanded three-year study to examine the effects of 10 repeated stimulations over two weeks.
Related Stories
The new study aims to build on initial findings by recruiting 120 participants with chronic insomnia. Over several months, participants will receive brief brain-stimulation sessions while their sleep is monitored through advanced trackers and at-home brain wave monitors.
“By investigating how different areas of the brain respond to continuous theta burst stimulation, we hope to fine-tune this approach for maximum effectiveness,” says Killgore. The goal is to determine whether the sleep improvements seen in the short term can be sustained following treatment.
Collaboration is key to this study’s design, as the team includes two active-duty military consultants with sleep disorders. Their input has been instrumental, ensuring the study’s relevance to military personnel and shaping plans for translating results into actionable changes for the military community.
This work aligns with Congress’ Traumatic Brain Injury and Psychological Health Research Program, specifically focusing on reducing psychological health risks and developing novel treatments. Dr. Jordan Karp, chair of the psychiatry department, believes this project could transform sleep science.
“This innovative project has tremendous potential to open new avenues for treating one of the major health concerns facing service members and the civilian community,” he says, highlighting its promise as a drug-free option for chronic insomnia and other sleep disorders.
As researchers proceed, they hold hope that continuous theta burst stimulation will become a practical, effective solution to the persistent problem of sleep deprivation in military contexts, helping to ensure the well-being and readiness of service members.
If successful, this treatment could offer new options not only for those in uniform but also for civilians struggling with sleep disorders.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Joshua Shavit
Science & Technology Writer | AI and Robotics Reporter
Joshua Shavit is a Los Angeles-based science and technology writer with a passion for exploring the breakthroughs shaping the future. As a contributor to The Brighter Side of News, he focuses on positive and transformative advancements in AI, technology, physics, engineering, robotics and space science. Joshua is currently working towards a Bachelor of Science in Business Administration at the University of California, Berkeley. He combines his academic background with a talent for storytelling, making complex scientific discoveries engaging and accessible. His work highlights the innovators behind the ideas, bringing readers closer to the people driving progress.