Light-induced gene therapy successfully kills cancer cells
Scientists develop a light-activated mitochondrial therapy that targets cancer cells, showing promise in treating glioblastoma and breast cancer.
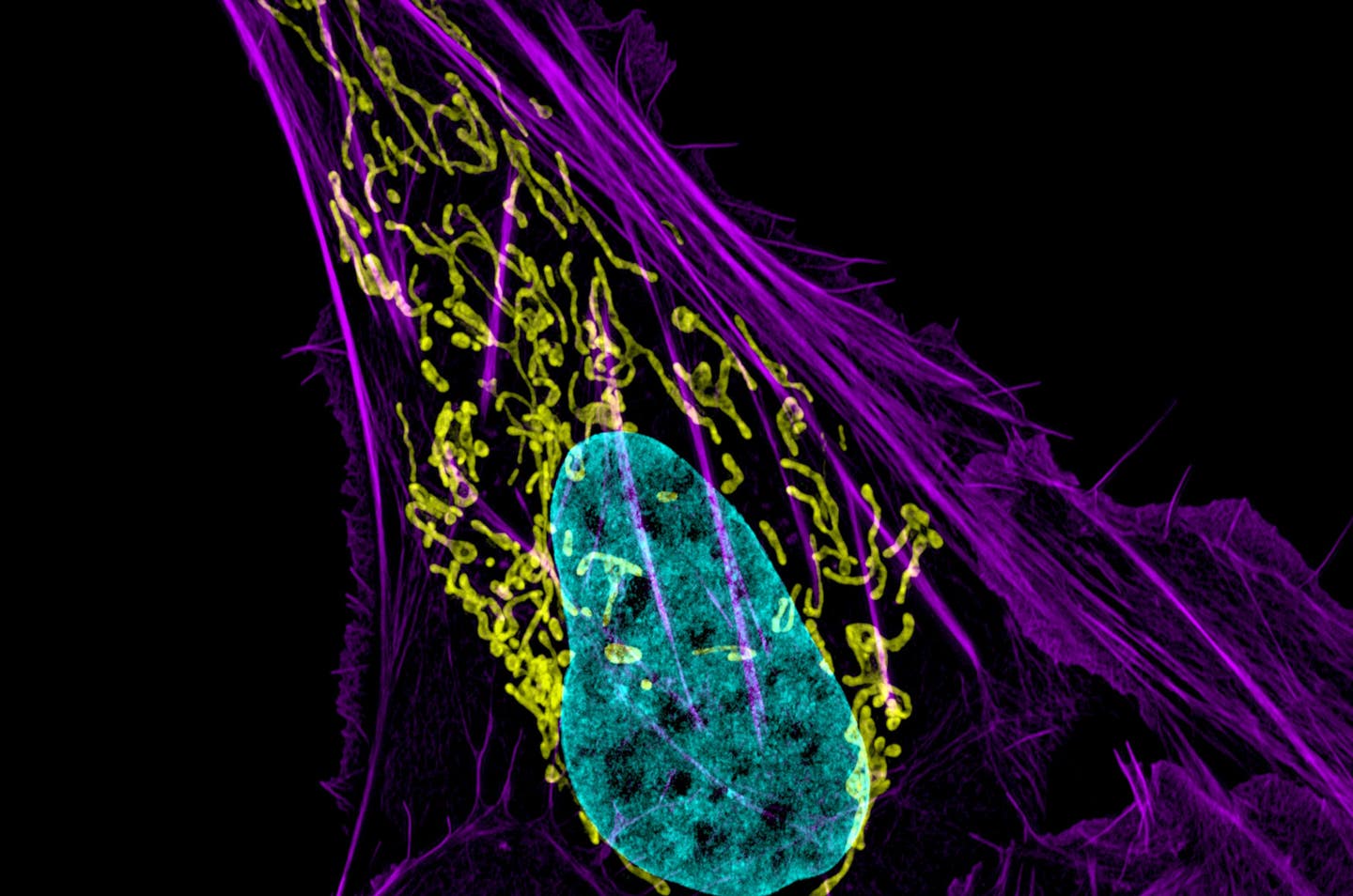
Researchers unveiled a groundbreaking mitochondrial therapy that uses internal bioluminescence to target and destroy cancer cells. (CREDIT: Dylan Burnette and Jennifer Lippincott-Schwartz, NICHD)
Mitochondria, the cell’s energy centers, play a vital role in regulating cellular processes, including growth and survival. Their unique structure and function have made them a promising target in the battle against cancer.
Mitochondrial genetics and metabolism are deeply involved in cancer progression—from aiding cell motility and invasion to modulating the tumor microenvironment. Despite these insights, developing mitochondrial-targeted therapies remains a challenge.
Numerous treatments targeting mitochondria, such as mitocans and mitochondriotoxics, aim to disrupt specific signaling pathways. These approaches often focus on proteins like hexokinase or Bcl2 family proteins. However, their long-term efficacy is limited due to the unpredictability of mutations in cancer cells. This has hindered the clinical success of mitochondrial therapies.
One innovative approach to tackling cancer involves targeting the inner mitochondrial membrane (IMM). Maintaining its electrical potential gradient, known as ∆Ψm, is critical for mitochondrial function. When ∆Ψm dissipates, it triggers cell death, making it a compelling target for cancer treatment.
Previous methods to disrupt ∆Ψm, such as chemical uncouplers or genetic modifications, often lacked specificity or caused irreversible side effects, limiting their utility.
A groundbreaking advancement in this field is mitochondrial optogenetics (mOpto). By introducing light-gated channelrhodopsins into mitochondria, researchers achieved controlled ∆Ψm depolarization and induced cell death. However, the need for external light sources to activate this mechanism limited its application to surface-level tumors.
Building on this, scientists have developed mitochondrial luminoptogenetics (mLumiOpto), which uses an internal light source. This approach combines cationic channelrhodopsin (CoChR), a protein activated by blue light, with nanoluciferase (NLuc), a bioluminescent enzyme.
The genes encoding these molecules are selectively expressed in cancer cells using a cancer-enhanced promoter. Once delivered to cancer cells, NLuc generates light that activates CoChR, causing mitochondrial collapse and cell death.
Related Stories
To deliver this gene therapy, researchers used a modified adeno-associated virus (AAV) combined with a monoclonal antibody. This delivery system ensures that the therapy targets cancer cells while sparing healthy tissue.
The virus is encapsulated in nanocarriers derived from human cells, enhancing its stability and effectiveness. The monoclonal antibody further improves specificity by binding to receptors on cancer cell surfaces.
The therapeutic potential of mLumiOpto was tested in preclinical mouse models of glioblastoma and triple-negative breast cancer. These aggressive cancers are notoriously difficult to treat. The results were promising.
In glioblastoma models, mLumiOpto significantly reduced tumor size and extended survival. Imaging studies confirmed that the effects were limited to cancerous tissues, with no detectable damage to healthy cells.
“We disrupt the membrane so mitochondria cannot work functionally to produce energy or work as a signaling hub. This causes programmed cell death followed by DNA damage – our investigations showed these two mechanisms are involved and kill the cancer cells,” explained Lufang Zhou, co-lead author and professor at The Ohio State University.
Zhou’s research team collaborated with X. Margaret Liu, a chemical engineering professor specializing in nanoparticle-based therapies. Together, they refined the AAV delivery system, ensuring its stability and cancer specificity.
Liu’s expertise in creating targeted anti-cancer therapies was instrumental in designing the delivery particles, which resemble naturally occurring extracellular vesicles in human blood. “This construction assures stability in the human body because this particle comes from a human cell line,” Liu noted.
Beyond its direct effects, the therapy also appears to stimulate the immune system. The monoclonal antibody triggers an immune response within the tumor microenvironment, potentially enhancing its therapeutic effects. This dual action—targeted cell death and immune activation—could prove invaluable in treating resistant cancers.
“Our approach targets mitochondria directly, using external genes to activate a process that kills cells. That’s an advantage, and we’ve shown we can get a very good result in killing different types of cancer cells,” Zhou said.
His team’s earlier studies had shown that disrupting the IMM’s electrical charge could be achieved using light-activated proteins. The mLumiOpto system builds on this by creating light from within the cells, making it viable for clinical use.
The researchers’ success lies not only in developing the therapy but also in proving its efficacy across multiple cancer types. In triple-negative breast cancer models, the treatment reduced tumor burden and prolonged survival. The technology’s versatility and precision make it a promising candidate for further research and clinical trials.
Ohio State University has filed a provisional patent for the mLumiOpto technology. The researchers continue to explore its applications in other cancers and refine its delivery mechanisms. Their work represents a significant step forward in the quest for targeted, minimally invasive cancer treatments.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Rebecca Shavit
Science & Technology Journalist | Innovation Storyteller
Based in Los Angeles, Rebecca Shavit is a dedicated science and technology journalist who writes for The Brighter Side of News, an online publication committed to highlighting positive and transformative stories from around the world. With a passion for uncovering groundbreaking discoveries and innovations, she brings to light the scientific advancements shaping a better future. Her reporting spans a wide range of topics, from cutting-edge medical breakthroughs and artificial intelligence to green technology and space exploration. With a keen ability to translate complex concepts into engaging and accessible stories, she makes science and innovation relatable to a broad audience.



