Lifesaving antibody treatment could revolutionize heart transplants
New research suggests there may be a way to further protect transplanted hearts from rejection with an anti-inflammatory antibody treatment before surgery occurs.
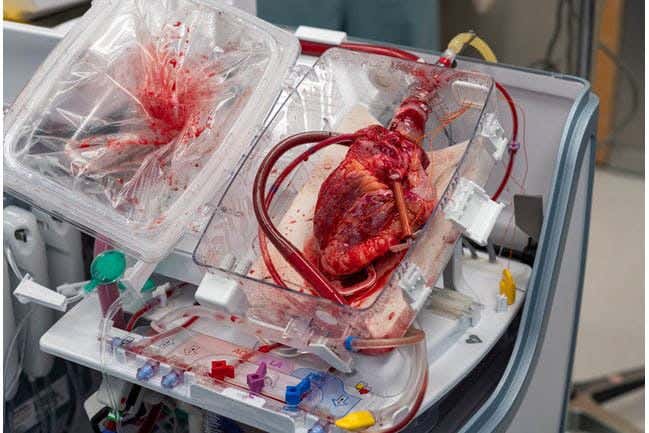
Heart transplant (CREDIT:
MUSC Health)
A new study by researchers at Cincinnati Children’s Hospital reveals a potential method to enhance the protection of transplanted hearts from rejection. By preparing both the donor organ and the recipient with an anti-inflammatory antibody treatment before surgery, scientists believe they can reduce the risk of rejection while preserving the body's ability to fight infections.
This research, published in PNAS, centers on blocking a specific immune response that typically occurs in reaction to microbial infections. This same immune response has been linked to harmful inflammation in transplanted hearts.
In mouse models, the study found that transplanted hearts remained functional for longer periods when the recipients received the novel antibody treatment. These findings mark the beginning of a complex journey to determine whether this approach could be safely applied to human heart transplants.
Dr. Chandrashekhar Pasare, DVM, PhD, who leads the Division of Immunobiology at Cincinnati Children’s, explains, “The anti-rejection regimens currently in use are broad immunosuppressive agents that make patients susceptible to infections. By using specific antibodies, we think we can just block the inflammation that leads to rejection but leave anti-microbial immunity intact.”
The research team, including first author Dr. Irene Saha, focused on how dendritic cells from the donor organ initiate an inflammatory response in the recipient. They discovered that memory CD4 T cells in the recipient activate these donor dendritic cells through signals sent by the proteins CD40L and TNFα. When this signaling pathway was blocked using gene editing techniques, the result was reduced inflammation and prolonged survival of the transplanted hearts.
In their experiments, untreated mice rejected the donated heart within a week. However, in mice genetically altered to lack receptors for CD40L and TNFα, the transplanted hearts maintained strong function through day 66, when the study concluded.
Related Stories
Pasare reflects on the significance of this discovery, stating, “We have been working on this for almost a decade. The major reason we figured out this pathway is that we focused on understanding how memory T cells in the recipient, with potential reactivity to donor-specific antigens, induce innate inflammation.
The rest of the field has focused on other concepts such as ischemia reperfusion injury, ligands from dead cells, and innate immune receptors, none of which seem to really lead to transplant rejection.”
He continues, “The key to preventing organ rejection is to take away the ability of the recipient’s memory T cells to initiate inflammation when they recognize donor antigens in dendritic cells. While T cell memory is critical to fight infections, the innate inflammation initiated by memory T cells is detrimental to the survival of transplanted organs.”
Looking ahead, the researchers are optimistic that the approach used to protect hearts from rejection could be applicable to other forms of organ transplantation. However, the gene editing techniques employed in the mouse models are not considered safe for human use. Therefore, the team is exploring alternative methods to disrupt the inflammatory response in humans.
“Using blocking antibodies against CD40 could be a good approach,” Pasare suggests. “Another option would be to create biologics or compounds that specifically target the TNF receptor superfamily in humans. I think this is a very exciting area for future drug development.”
This study opens the door to potentially safer and more effective ways to protect transplanted organs from rejection, signaling a promising direction for future research and therapeutic innovation.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Joshua Shavit
Science & Technology Writer | AI and Robotics Reporter
Joshua Shavit is a Los Angeles-based science and technology writer with a passion for exploring the breakthroughs shaping the future. As a contributor to The Brighter Side of News, he focuses on positive and transformative advancements in AI, technology, physics, engineering, robotics and space science. Joshua is currently working towards a Bachelor of Science in Business Administration at the University of California, Berkeley. He combines his academic background with a talent for storytelling, making complex scientific discoveries engaging and accessible. His work highlights the innovators behind the ideas, bringing readers closer to the people driving progress.



