Gut Microbes in Infancy Shape Diabetes Risk and Metabolic Health for Life
New research shows how gut microbes in infancy shape lifelong diabetes risk and pancreatic health through immune system interactions.
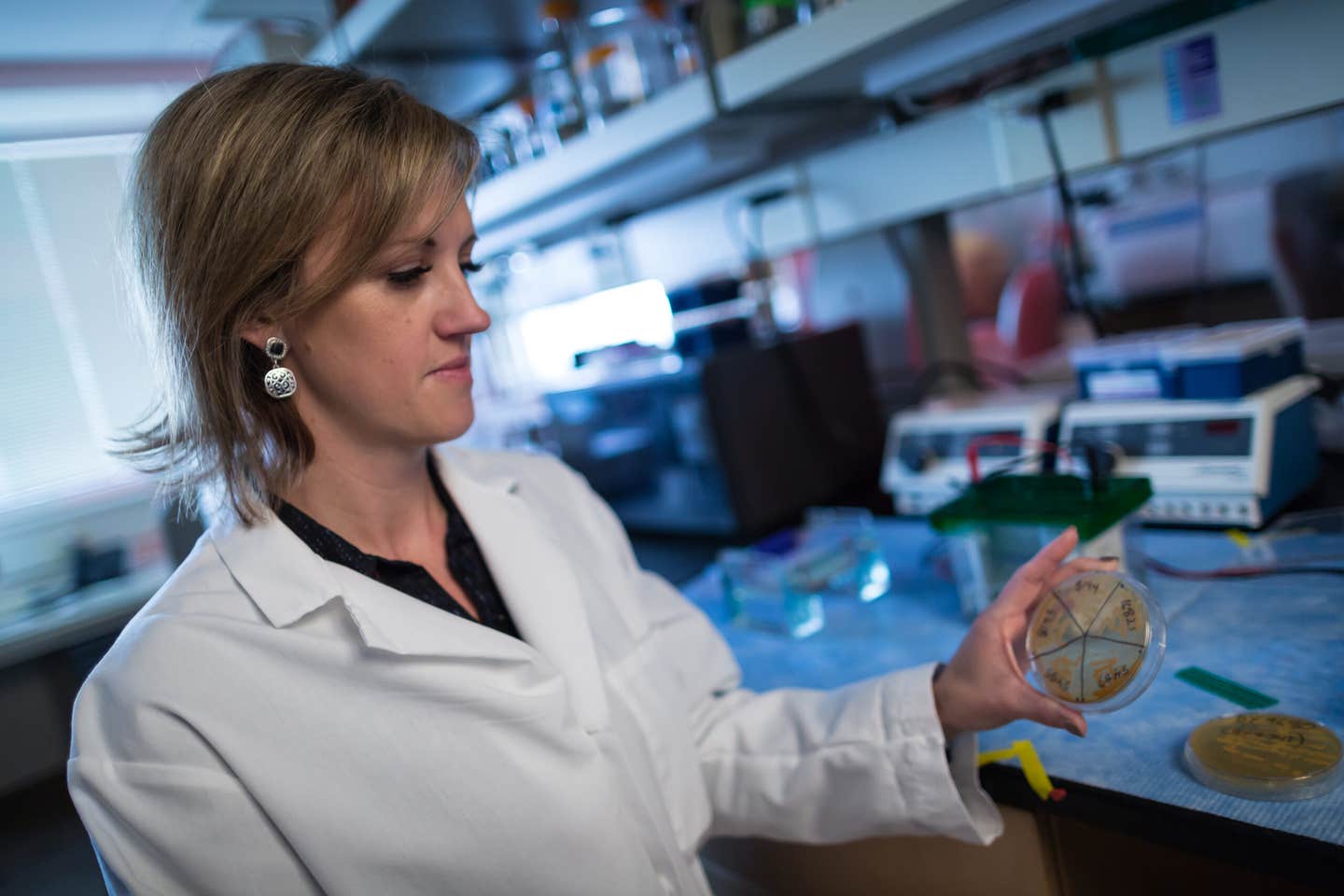
June Round inspects a dish of microbes cultured from the gut. (CREDIT: Charlie Ehlert / University of Utah Health)
From your first breath, trillions of tiny microbes colonize your body, shaping your health in surprising ways. Among these unseen residents, fungi and bacteria living in your gut play a crucial role in determining whether you might develop diabetes later in life.
Researchers have now uncovered how one unusual fungus, abundant in infancy but scarce in adulthood, can significantly affect your lifelong metabolic health.
Microbes and Your Pancreas: A Vital Connection
Your pancreas has specialized cells called beta cells, whose primary job is to produce insulin. Insulin helps control your blood sugar levels. Without enough beta cells or insulin, your risk for diabetes rises sharply.
Immediately after birth, your beta cells multiply quickly to meet the needs of your growing body. This rapid expansion phase sets the foundation for how many insulin-producing cells you'll have for life. Missing out on this early growth window can mean lifelong struggles with diabetes or poor metabolism.
Scientists already knew beta cells expanded rapidly after birth but didn't fully understand what triggered this growth. Now, researchers have identified gut microbes—especially certain fungi—as essential players during this critical period.
“Our findings show how important the microbiota is during this very short early period of development,” explains June Round, PhD, professor of pathology at the University of Utah Health. “This, to me, was shocking and a bit scary.”
A Window of Opportunity
To understand the link between microbes and pancreatic health, scientists examined newborn mice. They disrupted the mice’s gut microbiome by giving them antibiotics in the first 10 days after birth. Remarkably, mice treated during this brief window grew fewer beta cells. Later in life, these mice had consistently higher blood sugar levels, low insulin, and impaired metabolism—clear indicators of diabetes risk.
Related Stories
These experiments confirmed that the microbiome shapes beta cell development specifically during this narrow early-life period. If microbes were disrupted outside this window, beta cell growth wasn't significantly affected. Thus, timing is crucial.
But the researchers didn’t stop there. They pinpointed particular microbes that enhanced beta cell growth and insulin levels. One of these, an uncommon fungus named Candida dubliniensis, stood out for its powerful effects.
The Surprising Power of Fungi
Candida dubliniensis might seem an unlikely hero. In fact, it's rarely found in adults, and almost nothing was previously known about its health effects. Yet, researchers discovered it plays a major role in boosting beta cell growth and preventing diabetes in early life.
When scientists introduced C. dubliniensis to newborn mice, something remarkable happened. Male mice genetically prone to diabetes usually had a 90% chance of developing the disease. But when colonized with C. dubliniensis, fewer than 15% got diabetes. This striking result highlights the fungus’s potential to prevent diabetes altogether.
The researchers further tested if C. dubliniensis could help damaged beta cells regenerate in adult mice, a process previously thought impossible. Remarkably, even adult mice whose insulin-producing cells had been destroyed began regenerating beta cells when exposed to the fungus. Their insulin production improved, restoring normal metabolism.
“This kind of cell normally doesn't grow during adulthood,” emphasizes Jennifer Hill, PhD, the study's lead author, who conducted the research at the University of Utah and now teaches biology at the University of Colorado Boulder. “One possibility in the far future is that maybe signals like these could be harnessed not only as a preventative but also as a therapeutic to help later in life.”
Immune Cells: The Link to Diabetes Prevention
Why would a fungus like C. dubliniensis influence beta cells so strongly? The answer, researchers found, lies within your immune system—particularly specialized immune cells called macrophages.
Macrophages do more than just fight infections. They live in your pancreatic islets, closely interacting with beta cells. Researchers found that mice without microbiomes also had fewer macrophages in their pancreas. Introducing C. dubliniensis restored both macrophages and beta cell growth. Without these macrophages, the fungus had no benefit—indicating macrophages are essential intermediaries connecting microbes to metabolism.
“We're finding that these early-life signals do impact early development,” Hill explains, “and then have long-term consequences for metabolic health.”
From Mice to Humans: What Does This Mean for You?
While these results were initially observed in mice, scientists believe the process could be similar in humans. In infants, gut microbiomes naturally change over distinct phases. During these phases, beneficial microbes, including fungi like Candida, colonize your gut, influencing immune cells that support pancreatic health.
Notably, babies born through caesarean section miss out on early exposure to beneficial microbes, including fungi typically found in vaginal birth. Research links this absence to a higher risk of diabetes and other diseases. However, exposing caesarean-born infants to vaginal microbes immediately after birth may lower this risk.
These findings, published in the journal Science, also underscore the importance of microbial diversity. Studies indicate children lacking diverse gut microbes face greater diabetes risk, though scientists don't yet fully understand why. The discovery of C. dubliniensis offers clues, suggesting other microbes may also shape your metabolism profoundly.
Harnessing Microbes for Better Health
The ultimate goal is clear: identify beneficial microbes that doctors can provide early in life to prevent diabetes or even reverse pancreatic damage later in adulthood.
“Eventually, we're going to identify these important microbes,” Round says, “and we'll be able to give them to infants so that we can perhaps prevent this disease from happening altogether.”
However, researchers caution that treatments successful in mice don't always translate to humans. Still, their findings offer real hope. They illuminate how our earliest experiences with microbes set the stage for lifelong metabolic health. Future studies will determine if providing microbes like C. dubliniensis during infancy might effectively prevent diabetes in humans.
A New Path to Diabetes Prevention?
Though further research is needed, this discovery opens exciting possibilities. By identifying crucial microbial influences early in life, researchers may have found a groundbreaking way to prevent diabetes. It could even lead to revolutionary treatments capable of reversing pancreatic damage.
“We don’t know a lot about how the microbiome is impacting early-life health,” says Hill. “But we’re beginning to understand its huge potential.”
Your lifelong health could ultimately depend on the invisible microbes that first colonize your body. Understanding these microbes better might help doctors offer targeted treatments—changing the course of diabetes for generations to come.
Note: The article above provided above by The Brighter Side of News.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Joshua Shavit
Science & Technology Writer | AI and Robotics Reporter
Joshua Shavit is a Los Angeles-based science and technology writer with a passion for exploring the breakthroughs shaping the future. As a contributor to The Brighter Side of News, he focuses on positive and transformative advancements in AI, technology, physics, engineering, robotics and space science. Joshua is currently working towards a Bachelor of Science in Business Administration at the University of California, Berkeley. He combines his academic background with a talent for storytelling, making complex scientific discoveries engaging and accessible. His work highlights the innovators behind the ideas, bringing readers closer to the people driving progress.