Gum infection could be a major sign of heart trouble, study finds
Periodontitis, a gum disease, causes dental problems like bad breath, bleeding and tooth loss. Study found it’s linked to heart disease.
[Mar. 29, 2023: Norifumi Miyokawa, Hiroshima University]
Cysteamine could be used to prevent heart attacks and strokes due to clots. (CREDIT: Creative Commons)
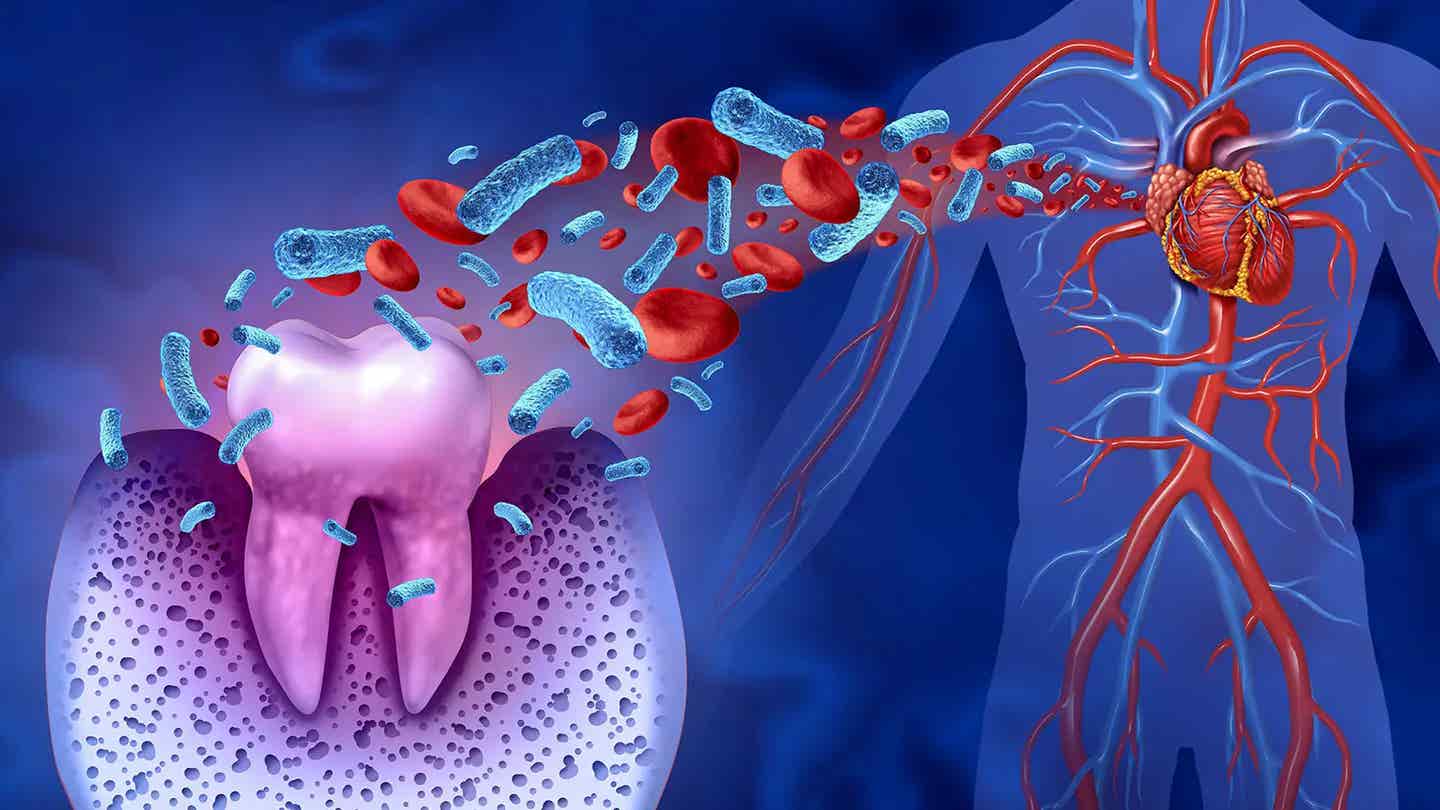
Periodontitis, a gum disease, can lead to a litany of dental issues from bad breath to bleeding and lost teeth. Now, researchers at Hiroshima University have found that it could be connected to even more severe problems elsewhere in the body — the heart.
In a study published in JACC: Clinical Electrophysiology, the team found a significant correlation between periodontitis and fibrosis — scarring to an appendage of the heart’s left atrium that can lead to an irregular heartbeat called atrial fibrillation — in a sample of 76 patients with cardiac disease.
“Periodontitis is associated with a long-standing inflammation, and inflammation plays a key role in atrial fibrosis progression and atrial fibrillation pathogenesis,” said first author Shunsuke Miyauchi, assistant professor with the Hiroshima University’s Health Service Center. He is also affiliated with the university’s Graduate School of Biomedical and Health Sciences.
“We hypothesized that periodontitis exacerbates atrial fibrosis. This histological study of left atrial appendages aimed to clarify the relationship between clinical periodontitis status and degree of atrial fibrosis.”
Related Stories
The left atrial appendages were surgically removed from the patients, and the researchers analyzed the tissue to establish the correlation between severity of the atrial fibrosis and severity of the gum disease. They found that the worse the periodontitis, the worse the fibrosis, suggesting that the inflammation of gums may intensify inflammation and disease in the heart.
“This study provides basic evidence that periodontitis can aggravate atrial fibrosis and can be a novel modifiable risk factor for atrial fibrillation,” said corresponding author Yukiko Nakano, professor of cardiovascular medicine in Hiroshima University’s Graduate School of Biomedical and Health Sciences.
According to Nakano, in addition to improving other risk factors such as weight, activity levels, tobacco and alcohol use, periodontal care could aid in comprehensive atrial fibrillation management. However, she cautioned that this study did not establish a causal relationship, meaning that while gum disease and atrial fibrosis degrees of severity appear connected, researchers have not found that one definitively leads to the other. “Further evidence is required for establishing that periodontitis contributes to the atrial fibrosis in a causal manner and that periodontal care can alter fibrosis,” Nakano said.
“One of our goals is to confirm that periodontitis is a modifiable risk factor for atrial fibrillation and to promote dental specialists’ participation in comprehensive atrial fibrillation management. Periodontitis is an easy modifiable target with lower cost among known atrial fibrillation risk factors. Thus, the achievement of this study series may bring benefits for many people worldwide.”
Andreas Goette, MD (St. Vincenz Hospital, Paderborn, Germany), who wrote an editorial accompanying the published study, notes that while the data suggest an association between periodontitis and atrial fibrosis, it does not demonstrate causation. Moreover, it is “unclear whether the release of inflammatory markers around infected teeth and oral tissue into the systemic circulation directly causes atrial changes . . .” or if other mechanisms are at play. Further studies “are now warranted to show that treatment of chronic periodontitis is atrial protective.”
Periodontal disease may be a risk factor for atrial fibrillation (AF) (CREDIT: Creative Commons)
In addition to that, Goette says the study “implies that chronic oral inflammation not only correlates to the histological finding of fibrosis, but also is directly related to clinical events like stroke.”
Symptoms of a Hearty Attack
According to the Mayo Clinic, symptoms of a heart attack vary. Some people have mild symptoms. Others have severe symptoms. Some people have no symptoms.
Common heart attack symptoms include:
Chest pain that may feel like pressure, tightness, pain, squeezing or aching
Pain or discomfort that spreads to the shoulder, arm, back, neck, jaw, teeth or sometimes the upper belly
Cold sweat
Fatigue
Heartburn or indigestion
Lightheadedness or sudden dizziness
Nausea
Shortness of breath
Women may have atypical symptoms such as brief or sharp pain felt in the neck, arm or back. Sometimes, the first symptom sign of a heart attack is sudden cardiac arrest.
Some heart attacks strike suddenly. But many people have warning signs and symptoms hours, days or weeks in advance. Chest pain or pressure (angina) that keeps happening and doesn't go away with rest may be an early warning sign. Angina is caused by a temporary decrease in blood flow to the heart.
For more science and technology stories check out our New Discoveries section at The Brighter Side of News.
Note: Materials provided above by Hiroshima University. Content may be edited for style and length.
Like these kind of feel good stories? Get the Brighter Side of News' newsletter.
Joseph Shavit
Head Science News Writer | Communicating Innovation & Discovery
Based in Los Angeles, Joseph Shavit is an accomplished science journalist, head science news writer and co-founder at The Brighter Side of News, where he translates cutting-edge discoveries into compelling stories for a broad audience. With a strong background spanning science, business, product management, media leadership, and entrepreneurship, Joseph brings a unique perspective to science communication. His expertise allows him to uncover the intersection of technological advancements and market potential, shedding light on how groundbreaking research evolves into transformative products and industries.



