Groundbreaking skin cancer treatment dramatically increases patient survival rates
By treating patients with a combination of two chemotherapy drugs, they were able to re-sensitize the cancer cells to ICB treatment.
[Nov. 22, 2022: Sam Cardwell, Hunter Medical Research Institute]
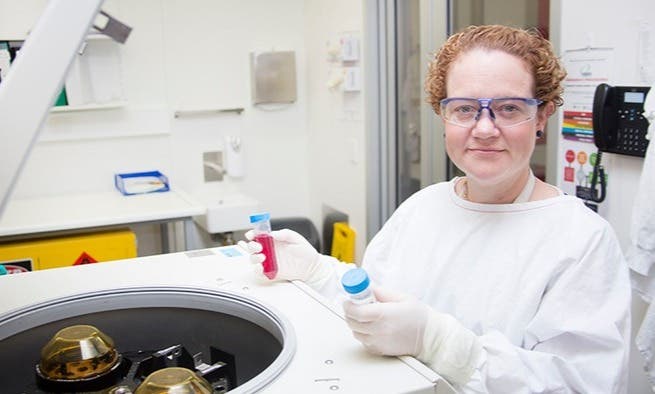
Professor Nikola Bowden in the lab at Hunter Medical Research Institute (Credit: Hunter Medical Research Institute)
HMRI and University of Newcastle researchers have discovered that treating patients who have late-stage treatment resistant melanoma with a combination of two existing drugs significantly increases their survival times.
Led by Professor Nikola Bowden and Dr Andre van der Westhuizen from HMRI’s Drug Repurposing and Medicines Research program, the project’s findings have been published in the American Association for Cancer Research journal Cancer Research Communications.
The drug repurposing trial focused on patients with end stage melanoma whose cancers had become resistant to frontline immunotherapy treatment, a class of drugs known as Immune Checkpoint Inhibiters (ICB). ICBs interfere with a cancer cells’ ability to ‘hide’ from the body's immune system allowing a patient’s own body to fight the cancer.
The team found that by treating patients with a combination of two already approved chemotherapy drugs, Azacitidine and Carboplatin, they were able to re-sensitize the cancer cells to ICB treatment.
Related Stories:
Professor Bowden said the study provided a potential new treatment for patients who, until now, had run out of options
“In this paper we have shown in a phase II study that treatment with Azacitidine and Carboplatin could be effective in priming for anti-immunotherapy (Avelumab) in patients with advanced ICB-resistant melanoma,” Professor Bowden said.
The team has been investigating these drugs since 2015 and, between 2017 and 2021, 20 patients, were given the two repurposed chemo drugs in order to ‘prime’ them for a subsequent immunotherapy treatment.
The patients survived an average of 47 weeks, with four of the patients still alive today following the treatment they received in the trial.
Tumor response, PFS, and OS. A, Spider plot of tumor burden change of target lesions in reference to the baseline tumor burden in 18 patients with measurable tumor burden. (Credit: Cancer Research Communications (2022))
“For some of the patients, it was like the tumors were frozen in time and they stayed the same for a very long time. Some patients even experienced a reduction in tumor size and number,” Professor Bowden said.
The drug repurposing trial was combined with a new form of immunotherapy.
Professor Nikola Bowden in the lab at Hunter Medical Research Institute (Credit: Image courtesy of Hunter Medical Research Institute)
Professor Bowden explains: “Melanoma cells send out a signal to the immune system that says, ‘I’m meant to be here’. The chemo drug combination we used mobilize the immune system to attack the tumors while the immunotherapy blocks that signal.”
This trial was initially funded by the Hunter Melanoma Foundation and generous community donations, including a $20,000 donation from the late Valerie Ryan.
The second stage of clinical trials are underway using updated immunotherapy drugs.
“Initial results suggest that this group of patients are doing even better on the new drugs,” Professor Bowden said.
Note: Materials provided above by Hunter Medical Research Institute. Content may be edited for style and length.
Like these kind of feel good stories? Get the Brighter Side of News' newsletter.
Joseph Shavit
Head Science News Writer | Communicating Innovation & Discovery
Based in Los Angeles, Joseph Shavit is an accomplished science journalist, head science news writer and co-founder at The Brighter Side of News, where he translates cutting-edge discoveries into compelling stories for a broad audience. With a strong background spanning science, business, product management, media leadership, and entrepreneurship, Joseph brings a unique perspective to science communication. His expertise allows him to uncover the intersection of technological advancements and market potential, shedding light on how groundbreaking research evolves into transformative products and industries.