Groundbreaking nanosurgical tool could lead to more effective cancer medications
This cutting-edge technology enabled researchers to observe individual cancer cells’ reactions to treatment and their evolution over time
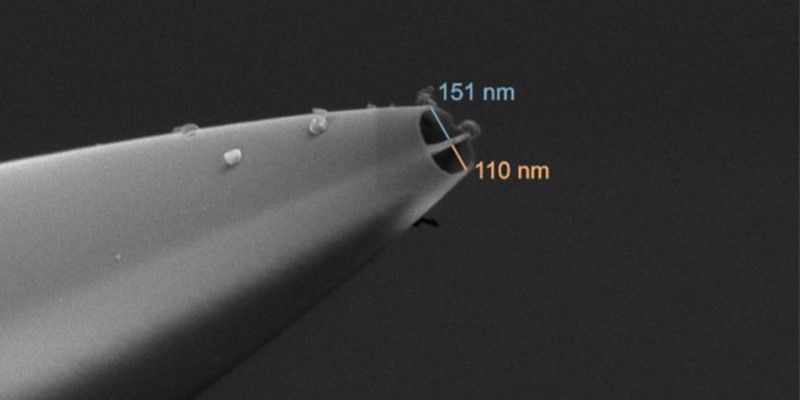
This cutting-edge technology has enabled researchers to observe individual cancer cells' reactions to treatment and their evolution over time. Electron microscopy image of the nanopipette. (CREDIT: Dr Alexander Kulak)
University of Leeds scientists have developed an advanced double-barrel nanopipette, which is now being utilized in the fight against cancer. This cutting-edge technology has enabled researchers to observe individual cancer cells' reactions to treatment and their evolution over time, potentially revolutionizing cancer medication development.
The nanopipette features two nanoscopic needles, allowing it to both inject and extract samples from the same cell simultaneously. Its semi-automated platform has drastically accelerated the process, facilitating the extraction of data from numerous individual cells with unprecedented accuracy and efficiency.
Traditionally, techniques for studying single cells often result in their destruction, limiting observations to either pre or post-treatment states. However, this new device can repeatedly biopsy living cells during cancer treatment without causing harm, enabling scientists to monitor their responses over time.
Electron microscopy image of the nanopipette. (CREDIT: Dr Alexander Kulak)
In a recent study published in the journal Science Advances, a multidisciplinary team comprising biologists and engineers investigated cancer cells' resistance to chemotherapy and radiotherapy using glioblastoma (GBM) as a model. GBM, the deadliest form of brain tumor, was chosen due to its notorious adaptability to treatment.
Dr. Lucy Stead, one of the study's corresponding authors and an Associate Professor of Brain Cancer Biology at the University of Leeds, emphasized the significance of this breakthrough. She noted that the technology provides a novel means to monitor changes in cells post-treatment, offering insights crucial for developing more effective cancer therapies.
GBM presents a particularly challenging case due to its resistance to existing treatments, leading to stagnant survival rates over the past two decades. Dr. Stead highlighted the importance of dynamically observing and characterizing these adaptable tumor cells to identify potential interventions.
Related Stories
Leading the Glioma Genomics research group at the Leeds Institute of Medical Research, Dr. Stead expressed optimism about the transformative potential of this technology in combating GBM, which remains an incurable disease.
Funded primarily by The Brain Tumour Charity, the research aims to improve understanding of GBM and develop more targeted treatments. Dr. Simon Newman, Chief Scientific Officer at The Brain Tumour Charity, emphasized the urgent need for effective treatments for this devastating disease.
The collaborative study involved researchers from various institutions, including Leeds' Bragg Centre for Materials Research, School of Electronic and Electrical Engineering, and the Earlham Institute in Norwich. Using the nanosurgical platform, the team meticulously analyzed single GBM cells over a 72-hour period.
Dr Lucy Stead, Associate Professor of Brain Cancer Biology in the University of Leeds’ School of Medicine. (CREDIT: University of Leeds)
Dr. Fabio Marcuccio, lead author of the study and a Research Associate at Imperial College London, highlighted the device's unprecedented precision in studying cancer cell adaptation to treatment over time. He underscored the collaborative effort and interdisciplinary approach essential for tackling complex challenges like cancer.
Cancer cell plasticity, the ability to adapt behavior, poses a significant obstacle in treatment, particularly in GBM. Understanding how these cells adapt and developing strategies to counteract their resistance could prevent cancer recurrence, offering hope to patients like Camilla Hawkins, diagnosed with GBM in 2022.
Illustration of the main phases of the single-cell nanobiopsy procedure. (CREDIT: Science Advances)
Dr. Paolo Actis, co-lead of the study and an Associate Professor of Bio-Nanotechnology at Leeds' School of Electronic and Electrical Engineering, emphasized the tool's ability to identify resilient cancer cells, crucial for developing targeted therapies.
Further research is needed to validate the technology's efficacy in both laboratory and clinical settings. Nonetheless, the insights gained thus far hold immense promise in advancing our understanding of cancer biology and improving patient outcomes.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get the Brighter Side of News' newsletter.
Joshua Shavit
Science & Technology Writer | AI and Robotics Reporter
Joshua Shavit is a Los Angeles-based science and technology writer with a passion for exploring the breakthroughs shaping the future. As a contributor to The Brighter Side of News, he focuses on positive and transformative advancements in AI, technology, physics, engineering, robotics and space science. Joshua is currently working towards a Bachelor of Science in Business Administration at the University of California, Berkeley. He combines his academic background with a talent for storytelling, making complex scientific discoveries engaging and accessible. His work highlights the innovators behind the ideas, bringing readers closer to the people driving progress.