Groundbreaking bioelectronic device fights infections without antibiotics
Researchers develop a bioelectronic device to manage infections without antibiotics, reducing biofilm formation and antibiotic resistance.
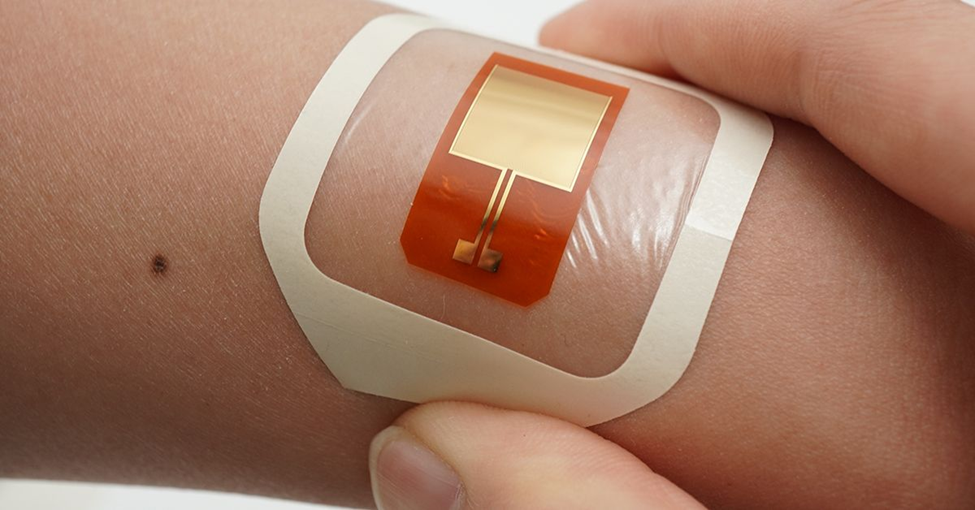
A new bioelectronic device developed by researchers taps into the natural electrical activity of bacteria to prevent infections. (CREDIT: University of Chicago)
Researchers from the University of Chicago and the University of California San Diego have taken a significant step forward in the fight against bacterial infections. The teams from the Bozhi Tian and Gürol Süel labs have developed a groundbreaking bioelectronic device, which taps into the natural electrical activity of bacteria found on human skin.
This innovative approach offers a drug-free method of managing infections, with the potential to address the growing issue of antibiotic resistance.
Published in DEVICE, the study reveals how programmable electrical stimulation can curb the harmful effects of Staphylococcus epidermidis, a common bacterium associated with hospital-acquired infections. This bacterium is also notorious for contributing to antibiotic resistance, a growing public health concern.
The device developed by the research teams features a flexible electroceutical patch that sends gentle electrical signals to the bacteria, preventing the formation of biofilms—clusters of bacteria that can lead to serious infections.
The implications of this research are vast, especially given the rising threat of antibiotic-resistant infections. Medical professionals estimate that drug-resistant infections could increase by 70% by 2050, making it more important than ever to find new solutions for managing bacterial infections. This bioelectronic device represents a promising alternative to traditional antibiotic treatments, especially as resistance to antibiotics continues to grow.
Related Stories
One of the key innovations of the device is its ability to target bacteria only in specific conditions. The patch activates bacterial responses only in acidic environments, mimicking the conditions found in healthy skin. This precise activation is important because it allows for the targeted treatment of infections without affecting the surrounding healthy tissue. The patch also reduces the virulence of the bacteria, meaning it lowers the activity of harmful genes without using antibiotics, further reducing the risk of developing resistance.
The research shows that the bioelectronic patch offers a localized treatment that limits the side effects often seen with antibiotic therapies. Because it can be applied directly to the affected area, the risk of systemic side effects is reduced.
In preclinical trials, the patch demonstrated impressive results, reducing bacterial colonization on pig skin by nearly tenfold. This suggests that the patch could be a powerful tool in preventing infections, particularly for patients with chronic wounds or those who have medical implants, where infections can be difficult to manage.
The ability to control bacterial behavior using electrical stimulation is a relatively new discovery. According to Gürol Süel, a professor at the UC San Diego School of Biological Sciences, the research team discovered action potentials in bacterial biofilms nearly a decade ago. This means that bacteria, long thought of as simple organisms, can be "excitable" and capable of behaviors similar to neurons in the brain.
Building on this insight, the collaboration between Süel's team and the Tian group led to the development of the wearable electroceutical device that can treat biofilm infections on the skin using electrical signals alone, without the need for antibiotics.
This innovative approach marks a new direction in bioelectronic medicine. The researchers are optimistic that the device could soon be used in clinical settings. For patients with chronic wounds or medical implants, this new method of infection control could provide more personalized and effective treatments, reducing the need for broad-spectrum antibiotics and minimizing the risk of resistance.
Looking ahead, healthcare professionals will need to explore how this research can be applied in infection control and other clinical settings. As the understanding of bacterial behavior continues to grow, so too does the potential for new treatments that harness the natural properties of bacteria to fight infections.
This device is a prime example of how science is evolving to meet the challenges posed by antibiotic resistance.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.