Genetically engineered muscle tissue can treat type 2 diabetes
Skeletal muscle tissue takes part in various functions in the body. It comprises about 40% of total body weight and provides stability.

[Oct 10, 2022: Judy Naylor, Diabetologia]
Skeletal muscle also plays a major role in glucose homeostasis, glycogen and lipid metabolism, and more. (CREDIT: Creative Commons)
Skeletal muscle tissue takes part in various functions in the body. It comprises about 40% of total body weight and provides stability and movement to the skeleton.
Skeletal muscle also plays a major role in glucose homeostasis, glycogen and lipid metabolism, and more. In recent years, the skeletal muscle tissue has been identified as a secretory organ; upon contraction, it releases muscle-specific cytokines and myokines that have local and/or systemic effects.
Skeletal muscle tissue is responsible for about 80% of infused glucose uptake. Skeletal muscle insulin resistance is a key defect in type 2 diabetes (T2D) and obesity.
The clinical guideline for T2D treatment is to normalize glycemia and thus minimize the chronic diabetes–related complications that can lead to medical disability, reduction in life expectancy, and high health costs.
Related Stories:
New tissue takes up more sugar from blood; hope is that a single injection of tissue could provide long-lasting glucose control, significantly improving quality of life and life expectancy.
Injections of genetically engineered muscle tissue hold great promise in treating type 2 diabetes (T2D), the annual meeting of the European Association for the Study of Diabetes in Stockholm, Sweden, will hear.
T2D is the most common form of diabetes and is responsible for more than 1 million deaths a year, globally.
Insulin resistance – where the body’s cells don’t respond properly to insulin and can’t easily take up glucose from blood, causing blood sugar levels to rise – is a key feature of T2D.
Over time, high blood sugar levels can damage the heart, eyes, feet and kidneys and shorten life expectancy by around ten years.
T2D is usually treated with oral medication and lifestyle changes initially but most people will need insulin injections eventually.
To find a better treatment, researchers at Levenberg Lab, Technion – Israel Institute of Technology genetically engineered muscle tissue to take up greater amounts of sugar from the blood.
In previous research, the transplantation of genetically engineered muscle cells into diabetic mice improved their blood sugar levels.1
“A single transplant of engineered tissue kept blood sugar levels lower for four months,” says researcher Ms Hagit Shoyhet.
In their latest research, the team used the same technique to genetically modify human muscle cells. The cells were engineered to make more insulin-activated sugar transporter (GLUT4), a protein that’s known to help cells take in sugar.
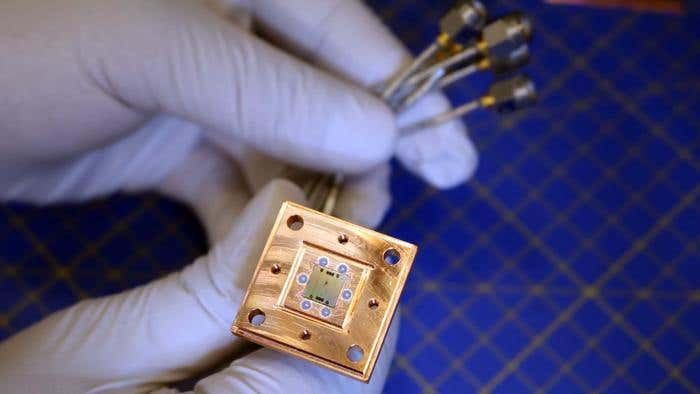
The cells were then grown into 3D tissue in the lab on scaffolds – matrices made from a biopolymer.
Tests showed that the new tissue was able to take up 50% more sugar than normal muscle tissue.
Pieces of tissue 6mm in diameter were then transplanted into diabetic mice through a small incision in the abdomen and their blood glucose levels were monitored.
The transplant resulted in a reduction in blood glucose levels of around 20%.
The team also developed a more flexible, sponge-like scaffold that could be injected using a syringe, removing the need for surgery.
The tissue grown on the new scaffold developed normally. Tests showed that injection did not cause significant damage to the tissue grown on the new scaffold and that the tissue could still take up sugar from the blood.
(A) Construct integration into the abdominal muscle of DIO mice 8 weeks after implantation. Scale bars, 5 and 2 mm. (B) Construct integration into the abdominal muscle of DIO mice 16 weeks after implantation. Scale bar, 0.5 mm. (C) Masson’s trichrome histology staining of implanted constructs 8 weeks after implantation. Scale bar, 200 μm; dashed line indicates the connection site between the construct (marked with C) and the tissue (marked with M for muscle). (D) Masson’s trichrome histology staining of implanted constructs 16 weeks after implantation. Scale bars, 200 μm; dashed line indicates the connection site between the construct (marked with C) and the tissue (marked with M for muscle). (CREDIT: Science Advances)
Ms Shoyhet says: “New treatments for type 2 diabetes are urgently needed. Our technique would allow a patient’s own cells to be modified to take up more glucose.
“Preliminary results indicate the approach has great potential and, in the future, a single injection of engineered tissue could provide long-lasting glucose control, significantly improving quality of life and life expectancy.”
The researchers have more pre-clinical work planned and hope to start clinical trials soon.
For more science and technology stories check out our New Discoveries section at The Brighter Side of News.
Note: Materials provided above by Diabetologia. Content may be edited for style and length.
Like these kind of feel good stories? Get the Brighter Side of News' newsletter.
Joseph Shavit
Head Science News Writer | Communicating Innovation & Discovery
Based in Los Angeles, Joseph Shavit is an accomplished science journalist, head science news writer and co-founder at The Brighter Side of News, where he translates cutting-edge discoveries into compelling stories for a broad audience. With a strong background spanning science, business, product management, media leadership, and entrepreneurship, Joseph brings a unique perspective to science communication. His expertise allows him to uncover the intersection of technological advancements and market potential, shedding light on how groundbreaking research evolves into transformative products and industries.