First-ever study reveals the impact of weight loss and blood sugar control on Type 2 diabetes
The study is the first of its kind to assess the real-world impacts of these medications on clinical outcomes, revealing significant findings for cardiovascular and kidney health.

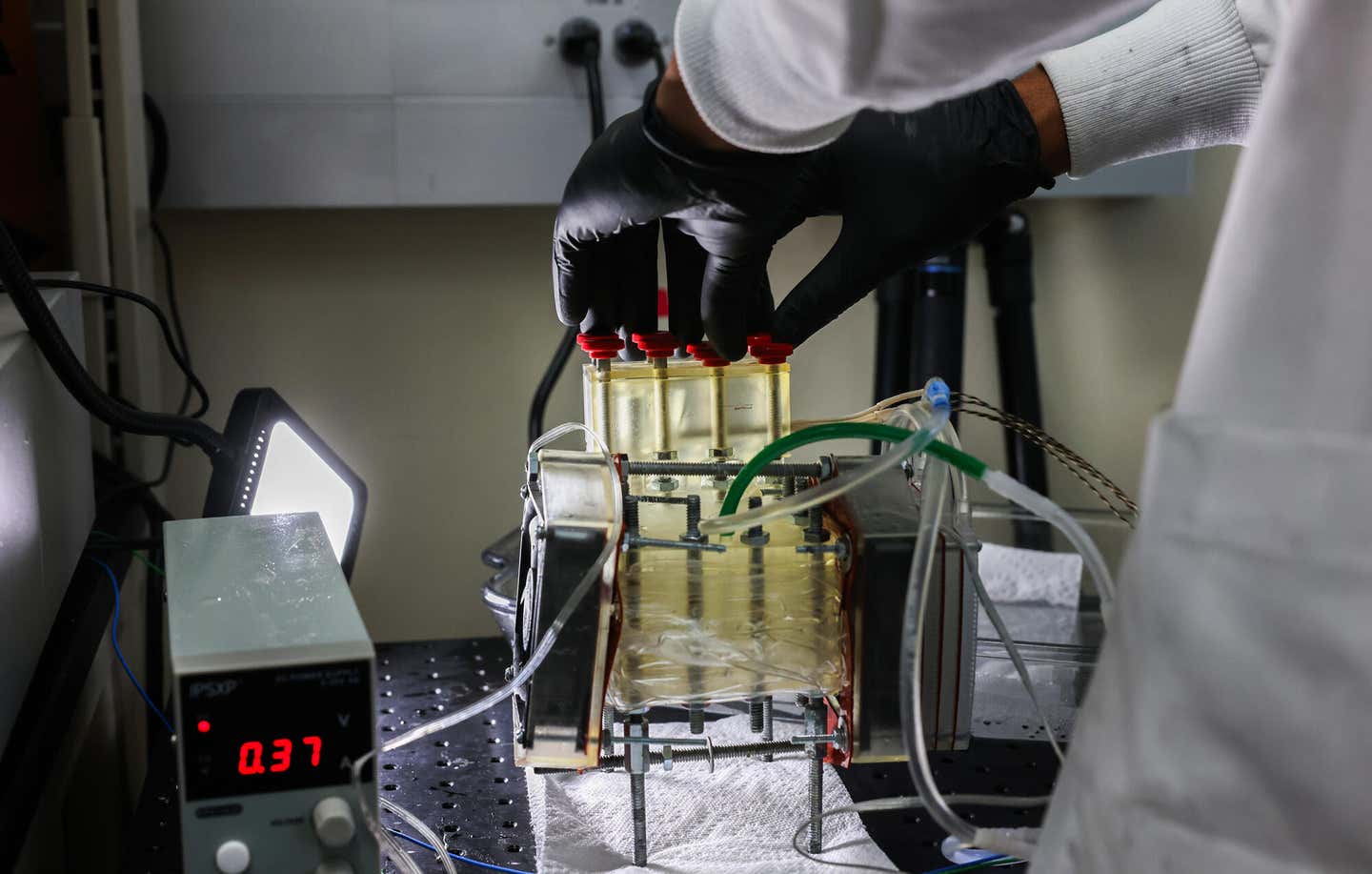
Managing diabetes isn’t a one-size-fits-all solution, and the interplay between blood sugar control, body weight, and health outcomes is complex. (CREDIT: CC BY-SA 3.0)
A groundbreaking study from the Cleveland Clinic sheds new light on the independent effects of weight loss and blood sugar control in people with type 2 diabetes (T2D) treated with antidiabetic medications, specifically those taking GLP-1 receptor agonists (GLP-1RAs), a class that includes well-known drugs like Ozempic and Wegovy.
The study is the first of its kind to assess the real-world impacts of these medications on clinical outcomes, revealing significant findings for cardiovascular and kidney health.
One of the study’s key discoveries is that for every 1% decrease in body mass index (BMI), there’s a corresponding 4% decrease in cardiovascular disease (CVD) risk. This benefit occurs even if blood sugar levels remain unchanged.
Conversely, better blood sugar control—independent of weight loss—was linked to a lower risk of chronic kidney disease (CKD). These results emphasize the importance of addressing both weight management and blood sugar levels in patients with type 2 diabetes.
Managing diabetes isn’t a one-size-fits-all solution, and the interplay between blood sugar control, body weight, and health outcomes is complex. However, weight loss, even in small amounts, has been shown to reduce cardiovascular risks and improve outcomes for people with T2D.
Losing just 5%–10% of body weight can have a positive impact on factors like blood pressure, triglyceride levels, and high-density lipoprotein (HDL) cholesterol levels within just a year. Unfortunately, many traditional antidiabetic medications have a known side effect: weight gain. But newer drugs like GLP-1RAs offer the potential for both blood sugar control and weight loss, reshaping how T2D is treated.
Related Stories
Despite the promise of these medications, there is still a wide variation in how much weight people lose, even when their glycated hemoglobin (HbA1c) levels—an indicator of blood sugar control—are well managed. Clinical trials have demonstrated that GLP-1RAs can reduce cardiovascular risks, but this study is one of the few to evaluate their effects in a real-world setting.
This research took advantage of Cleveland Clinic’s electronic health record (EHR) system to explore how weight loss and blood sugar control, when achieved through antidiabetic medications, affect patient outcomes. The goal was to clarify the independent contributions of these factors to health, particularly for those using GLP-1RAs. This real-world data offers new insights that can help improve the clinical management of T2D.
The study found that in patients treated with various antidiabetic medications, a reduction in BMI one year after starting treatment significantly lowered the risk of heart failure, hypertension, and the need for insulin. Meanwhile, HbA1c reduction was also associated with a lower risk of hypertension and insulin use. Consistent weight loss and blood sugar reduction were particularly linked to delaying the need for insulin.
In those starting on GLP-1RAs, the results were even more promising. Weight loss reduced the risks of cardiovascular disease, osteoarthritis, and the need for insulin, similar to the effects seen in patients using other antidiabetic drugs. Additionally, lower HbA1c levels were associated with a reduced risk of CKD and insulin use, regardless of weight loss.
Interestingly, the reduction in CVD and CKD risk was only linked to changes in BMI and HbA1c in patients using GLP-1RAs. This suggests that while weight loss is critical, the benefits of these drugs may extend beyond weight management. In fact, other studies have suggested that weight loss following bariatric surgery, which is not tied to GLP-1RA use, also reduces the risk of CVD and CKD. Thus, weight loss, in general, is likely a significant contributor to improved health outcomes.
A critical takeaway is that maintaining weight loss can help prevent many obesity-related conditions, which is particularly important for those with diabetes. In addition to lowering cardiovascular risks, weight loss and blood sugar control reduce the likelihood of developing hypertension, osteoarthritis, and insulin dependence. Even small fluctuations in BMI and HbA1c levels were linked to health risks, further underscoring the need for consistent management of weight and blood sugar levels.
People with T2D often struggle with weight loss, which can be challenging given the nature of the disease and its associated treatments. This makes the role of drugs like GLP-1RAs especially important, as they provide both weight loss and blood sugar control benefits. Given the strong association between diabetes, obesity, and cardiovascular disease—the leading cause of death in diabetic patients—any treatment that can tackle both issues is worth considering.
In addition to cardiovascular disease, obesity and diabetes are linked to osteoarthritis and musculoskeletal pain, which can significantly affect quality of life. The study demonstrated that controlling weight and blood sugar independently reduced the risks of these comorbidities. However, different GLP-1RA medications may have varying effects on specific conditions.
For instance, drugs like liraglutide, dulaglutide, and semaglutide have shown superior cardiovascular benefits, which may be due to their ability to reduce atherosclerosis, the underlying cause of many cardiovascular problems. Further studies are needed to explore how these drugs affect different comorbidities, even within the same drug class.
Animal studies provide additional insight into the mechanisms behind obesity-related diseases. Recent research in mice shows that a high-fat diet can disrupt lipid metabolism, leading to oxidative stress and damage to important proteins. These findings may help scientists identify potential diagnostic targets for conditions like cardiovascular disease in people with obesity.
Other studies suggest that the link between obesity and hypertension may be due to a combination of factors, including oxidative stress, kidney damage, and insulin resistance. These insights could lead to new precision therapies targeting specific disease pathways.
While this study offers valuable insights, it does have limitations. The sample size was constrained by the number of patients within the EHR who received specific drugs, and some clinical outcomes were only coded for billing purposes, which might not capture the full picture. Additionally, the study’s median follow-up period of five years might not be long enough to fully understand the long-term effects of weight loss and blood sugar control.
The findings provide real-world evidence that weight loss, independent of blood sugar control, can significantly reduce the risk of cardiovascular disease, while better blood sugar management can lower the risk of chronic kidney disease. These results support the continued use of GLP-1 receptor agonists in diabetes care and offer valuable guidance for doctors and patients aiming to improve long-term health outcomes.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Joshua Shavit
Science & Technology Writer | AI and Robotics Reporter
Joshua Shavit is a Los Angeles-based science and technology writer with a passion for exploring the breakthroughs shaping the future. As a contributor to The Brighter Side of News, he focuses on positive and transformative advancements in AI, technology, physics, engineering, robotics and space science. Joshua is currently working towards a Bachelor of Science in Business Administration at the University of California, Berkeley. He combines his academic background with a talent for storytelling, making complex scientific discoveries engaging and accessible. His work highlights the innovators behind the ideas, bringing readers closer to the people driving progress.