First-ever 3D treatment can revolutionize diabetes care
Researchers at Queen’s University Belfast have designed a new bandage treatment, known as a scaffold, to treat diabetic foot ulcers.
[Oct 9, 2022: Suzanne Lagan, Queen's University Belfast]
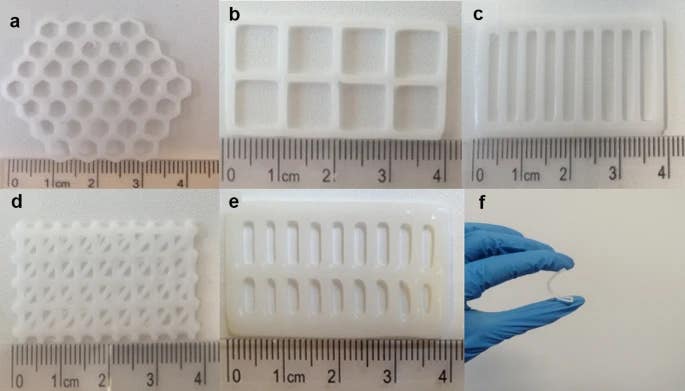
Digital images showing honeycomb (a), square (b), parallel (c), triangular (d), double-parallel (e), and the flexibility of a bioprinted PCL scaffold (f). (CREDIT: SpringerLink)
Researchers at Queen’s University Belfast have designed a new bandage treatment, known as a scaffold, to treat diabetic foot ulcers, which is cost-effective while improving patient outcomes. Produced by 3D bioprinting, the scaffolds slowly release antibiotics over a four-week period to effectively treat the wound.
Diabetes, a lifelong condition that causes a person's blood sugar level to become too high, is among the top ten causes of deaths worldwide.
Diabetic foot ulcer (DFU), is a serious complication of diabetes, affecting approximately 25% of diabetic patients. When identified, over 50% are already infected and over 70% of cases result in lower limb amputation.
The treatment strategy required for the effective healing of DFU is a complex process that requires several combined therapeutic approaches. As a result, there is a significant clinical and economic burden associated in treating DFU. These treatments are often unsuccessful, which leads to lower-limb amputation.
Related Stories:
This new research demonstrates outcomes with significant implications for patient quality of life, as well as decreasing the costs and clinical burden in treating DFU.
Recent research has focused on drug-loaded scaffolds to treat DFU. The scaffold structure is a novel carrier for cell and drug delivery that enhances wound healing.
The research, published in Springer Link, will be presented by Professor Lamprou at the Controlled Release Society (CRS) Workshop Italy.
This proof of concept study demonstrates the innovative potential of bioprinting technologies in fabrication of antibiotic scaffolds for the treatment of DFU. (CREDIT: SpringerLink)
Professor Dimitrios Lamprou, a Professor of Biofabrication and Advanced Manufacturing at Queen's School of Pharmacy and corresponding author, explains: “These scaffolds are like windows that enable doctors to monitor the healing constantly. This avoids needing to remove them constantly, which can provoke infection and delay the healing process.
“The ‘frame’ has an antibiotic that helps to ‘kill’ the bacteria infection, and the ‘glass’ that can be prepared by collagen/sodium alginate can contain a growth factor to encourage cell growth. The scaffold has two molecular layers that both play an important role in healing the wound.”
SEM micrographs of PCL control scaffolds, showing honeycomb (a), square (b), parallel (c), triangular (d), double-parallel (e), and a 3.0% LFX-loaded scaffold (f). All images were taken at × 50 magnification. (CREDIT: SpringerLink)
Lead author Ms Katie Glover, from the Queen’s School of Pharmacy, concludes: “Using bioprinting technology, we have developed a scaffold with suitable mechanical properties to treat the wound, which can be easily modified to the size of the wound. This provides a low-cost alternative to current DFU treatments, which could revolutionise DFU treatment, improving patient outcomes while reducing the economic burden caused by rapidly increasing patient demand as the number of people with diabetes continues to increase every year.”
Conclusions
The proof of concept study outlines the capabilities of bioprinting technologies to produce scaffolds able to provide sustained release of antibiotic to infected DFU.
Schematics showing a extrusion-based, b inkjet-based, and c laser-assisted bioprinting technologies. (CREDIT: SpringerLink)
In the study, the chosen scaffold design demonstrated suitable mechanical properties for tissue engineering purposes and can be easily modified to the size of the wound.
Moreover, the study has provided a simplified, low-cost alternative to current DFU treatments, which are often unsuccessful and incur significant costs, thus demonstrating the potential of bioprinting to revolutionise DFU treatment.
In future directions, it would be interesting to include in the scaffold a further layer with the purpose to provide dual administration of therapeutics through inclusion of drugs, cells, or biologics. Overall, this approach would act to simplify the current DFU treatment strategy, thus reducing the economic burden caused by rapidly increasing patient demand.
For more science and technology stories check out our New Discoveries section at The Brighter Side of News.
Note: Materials provided above by Queen's University Belfast. Content may be edited for style and length.
Like these kind of feel good stories? Get the Brighter Side of News' newsletter.
Joseph Shavit
Head Science News Writer | Communicating Innovation & Discovery
Based in Los Angeles, Joseph Shavit is an accomplished science journalist, head science news writer and co-founder at The Brighter Side of News, where he translates cutting-edge discoveries into compelling stories for a broad audience. With a strong background spanning science, business, product management, media leadership, and entrepreneurship, Joseph brings a unique perspective to science communication. His expertise allows him to uncover the intersection of technological advancements and market potential, shedding light on how groundbreaking research evolves into transformative products and industries.



