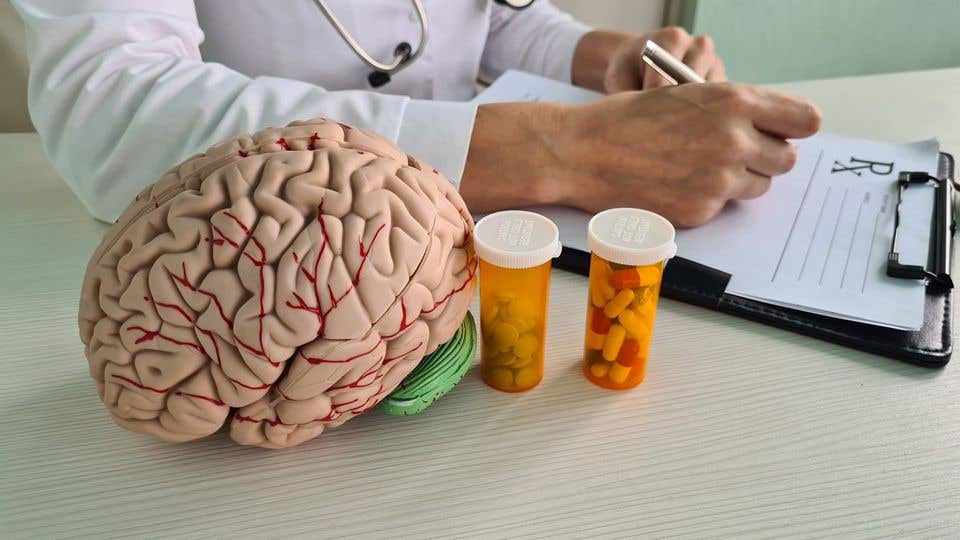
FDA-approved antidepressant shown effective at treating brain tumors
Vortioxetine, an antidepressant, shows promise in treating glioblastoma. Scientists hope clinical trials will confirm its effectiveness in humans, offering new hope for patients battling this aggressive brain tumor.
Vortioxetine: A New Hope for Glioblastoma Treatment. (CREDIT: CC BY-SA 3.0)
Glioblastoma, a highly aggressive form of brain cancer, remains an incurable disease despite advancements in medical treatment. While doctors can use surgery, radiation, and chemotherapy to extend the lives of patients, the prognosis is bleak—half of all patients succumb to the disease within a year of diagnosis. This has driven neuro-oncologists to search urgently for new drugs capable of targeting brain tumors more effectively.
One of the major challenges in treating brain tumors like glioblastoma is the difficulty of finding drugs that can cross the blood-brain barrier. This natural defense mechanism protects the brain by preventing harmful substances from entering, but it also limits the range of potential treatments for brain-related diseases. To address this, researchers have been exploring new possibilities for drugs that can successfully bypass this barrier and target tumor cells.
Recently, a team of researchers led by ETH Zurich Professor Berend Snijder has made a promising discovery. Through extensive laboratory work, they identified vortioxetine, an antidepressant, as an effective drug against glioblastoma. Vortioxetine, which is already approved by the FDA in the U.S. and Swissmedic, has the crucial ability to cross the blood-brain barrier, making it a valuable candidate for further study in treating brain tumors.
Sohyon Lee, the lead author of the study and a postdoctoral researcher in Snijder’s lab, played a pivotal role in this discovery. She utilized a cutting-edge drug-screening platform called pharmacoscopy, which was developed at ETH Zurich over the past several years. The team published their findings in the prestigious journal Nature Medicine, working in collaboration with neurologists Michael Weller and Tobias Weiss from the University Hospital Zurich (USZ).
A Revolutionary Screening Technique
Pharmacoscopy is a powerful screening platform that allows researchers to simultaneously test hundreds of active substances on living cells taken from human cancer tissue.
Related Stories:
In this study, the researchers focused primarily on neuroactive drugs, such as antidepressants, Parkinson’s medications, and antipsychotics, which have the ability to cross the blood-brain barrier. Over the course of the study, the ETH Zurich team tested approximately 130 different compounds on tumor tissue samples collected from 40 glioblastoma patients.
Using advanced imaging techniques and computer analysis, the researchers were able to observe the effects of these substances on cancer cells. Pharmacoscopy had previously been used by Snijder's team to study blood cancer, but this was the first time it had been applied to solid tumors like glioblastomas. The platform's capabilities allowed them to identify which drugs showed promise in fighting the tumor cells.
Lee's work involved analyzing fresh tumor tissue samples from patients who had recently undergone surgery at the University Hospital Zurich. These samples were then processed in the lab and screened on the pharmacoscopy platform. Within two days, the researchers could determine which drugs were effective and which were not.
Unexpectedly Potent Antidepressants
The results were surprising. Some of the antidepressants tested had a significant impact on glioblastoma cells, though not all of them were effective. The drugs that worked did so by triggering a rapid signaling cascade—a process that is vital for neuronal progenitor cells but also suppresses cancer cell division. Of all the drugs tested, vortioxetine stood out as the most effective in disrupting the tumor cells.
To further explore these findings, the ETH Zurich researchers ran computer simulations, testing over a million substances for their potential effectiveness against glioblastoma. Their simulations confirmed that the interplay between the signaling pathways in neurons and cancer cells was key to understanding why certain neuroactive drugs, like vortioxetine, could combat the tumor while others could not.
In an additional step, researchers at the University Hospital Zurich conducted trials using vortioxetine on mice with glioblastoma. The antidepressant showed promising results in these preclinical trials, particularly when used in combination with the current standard treatments.
Looking Ahead: Clinical Trials and New Hope
Following these promising lab results, the research team is now preparing to move forward with clinical trials. Two trials are planned: one will test the efficacy of vortioxetine in glioblastoma patients in combination with existing treatments such as surgery, radiation, and chemotherapy. The other will involve a personalized approach, where patients receive a drug regimen tailored specifically to them based on results from the pharmacoscopy platform.
One major advantage of vortioxetine is its availability and affordability. “The advantage of vortioxetine is that it is safe and very cost-effective,” says Michael Weller, Professor of Neurology at the University Hospital Zurich and coauthor of the study.
Because the drug is already approved for use, it won’t need to go through the lengthy approval process that new drugs often face, potentially speeding up its availability for glioblastoma patients. Weller is optimistic about the drug’s potential to become part of the standard therapy for this deadly form of cancer, but he also advises caution.
Patients and their families are urged not to seek out vortioxetine independently, as its effectiveness in humans remains unproven, and the appropriate dosage for treating glioblastoma has yet to be determined. Weller emphasizes the importance of conducting clinical trials before recommending it as a treatment. “Self-medicating would be an incalculable risk,” he warns.
Snijder echoes this sentiment, stating, “So far, it’s only been proven effective in cell cultures and in mice.” Despite these precautions, he believes that their research has yielded a critical breakthrough. “We started with this terrible tumor and found existing drugs that fight against it. We show how and why they work, and soon we’ll be able to test them on patients.”
Should vortioxetine prove effective in humans, it would mark a significant development in the fight against glioblastoma, offering new hope for patients battling this devastating disease.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.