Breakthrough vaccine found to protect people with HIV
HBV is spread primarily through sexual contact and sharing of contaminated needles. It causes chronic hepatitis B infection & liver disease.
[Oct 23, 2022: Kathy Stover, NIH/National Institute of Allergy and Infectious Diseases]
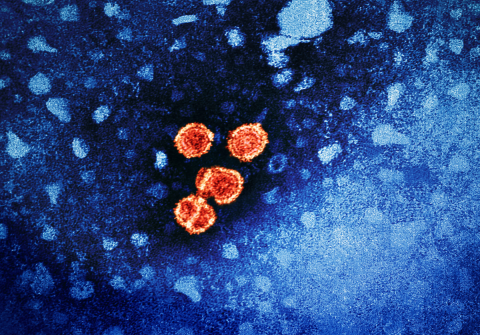
Hepatitis B virus particles (red) (CREDIT: CDC/NIAID)
A three-dose course of the hepatitis B vaccine HEPLISAV-B fully protected adults living with HIV who had never been vaccinated against or infected with the hepatitis B virus (HBV), according to study findings presented at the IDWeek conference in Washington, D.C. The National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, sponsors the ongoing Phase 3 ACTG A5379 clinical study.
HBV is spread primarily through sexual contact and sharing of contaminated needles. It causes chronic hepatitis B infection and can lead to progressive liver disease.
People living with HIV, including those who are taking antiretroviral therapy, are at greater risk of liver-related illness and death when co-infected with HBV. According to the Centers for Disease Control and Prevention, 10% of U.S. adults with HIV also have hepatitis B. People living with HIV are less likely to produce a protective immunological response to HBV vaccination.
The HEPLISAV-B vaccine, made by the Dynavax Technologies Corp. based in Emeryville, California, was approved in 2017 by the U.S. Food and Drug Administration as a two-dose vaccine regimen for adults. However, little was known about its protective effects in people living with HIV.
Related Stories:
Led by study chairs Kenneth E. Sherman, M.D., Ph.D., of the University of Cincinnati College of Medicine, and Kristen Marks, M.D., of Weill Cornell Medical College, New York City, the researchers tested a three-dose course of HEPLISAV-B among 68 adults living with HIV at 38 sites in the United States, South Africa, and Thailand.
None of the participants had received a previous HBV vaccination or had evidence of a previous HBV infection; all were on antiretroviral therapy. Following the initial dose of HEPLISAV-B vaccine 0.5 milliliter (mL) as an intramuscular injection, study participants received additional doses at four weeks and 24 weeks.
The objective of this part of the study was to assess anti-HBV surface antibodies (HBsAbs) greater than or equal to 10 milli-international units per milliliter (mIU/mL) at week 28 (defined as seroprotection from HBV) and to assess the vaccine’s safety.
Kenneth Sherman, M.D., Ph.D., is shown in the University of Cincinnati College of Medicine. (CREDIT: University of Cincinnati College of Medicine)
All participants achieved seroprotection with 88% of participants achieving HbsAb levels greater than 1000 mIU/mL, according to findings presented today. High antibody levels are thought to be associated with long-term vaccine durability.
At eight weeks after the second dose, 94.4% of participants achieved seroprotection; this percentage increased to 98.5% by week 24 prior to the third dose. The most common side effects related to vaccination were injection site pain, malaise, fatigue, muscle aches and headaches.
Kristen Marks, M.D., of Weill Cornell Medical College, New York City (CREDIT: Cornell University)
The international study will continue to examine the effects of two-dose HEPLISAV-B, as well as a three-dose regimen of another hepatitis B vaccine (ENGERIX-B, manufactured by GSK) among adult participants with HIV who were previously vaccinated against HBV but who did not achieve an adequate immunologic response.
The clinical trial is estimated to complete vaccinations in March 2023.
Note: Materials provided above by NIH/National Institute of Allergy and Infectious Diseases. Content may be edited for style and length.
Like these kind of feel good stories? Get the Brighter Side of News' newsletter.
Joseph Shavit
Head Science News Writer | Communicating Innovation & Discovery
Based in Los Angeles, Joseph Shavit is an accomplished science journalist, head science news writer and co-founder at The Brighter Side of News, where he translates cutting-edge discoveries into compelling stories for a broad audience. With a strong background spanning science, business, product management, media leadership, and entrepreneurship, Joseph brings a unique perspective to science communication. His expertise allows him to uncover the intersection of technological advancements and market potential, shedding light on how groundbreaking research evolves into transformative products and industries.