Breakthrough studies look to predict migraine headaches
A study examines why some adolescent girls develop migraine headaches and others do not and how puberty plays a role in that development.
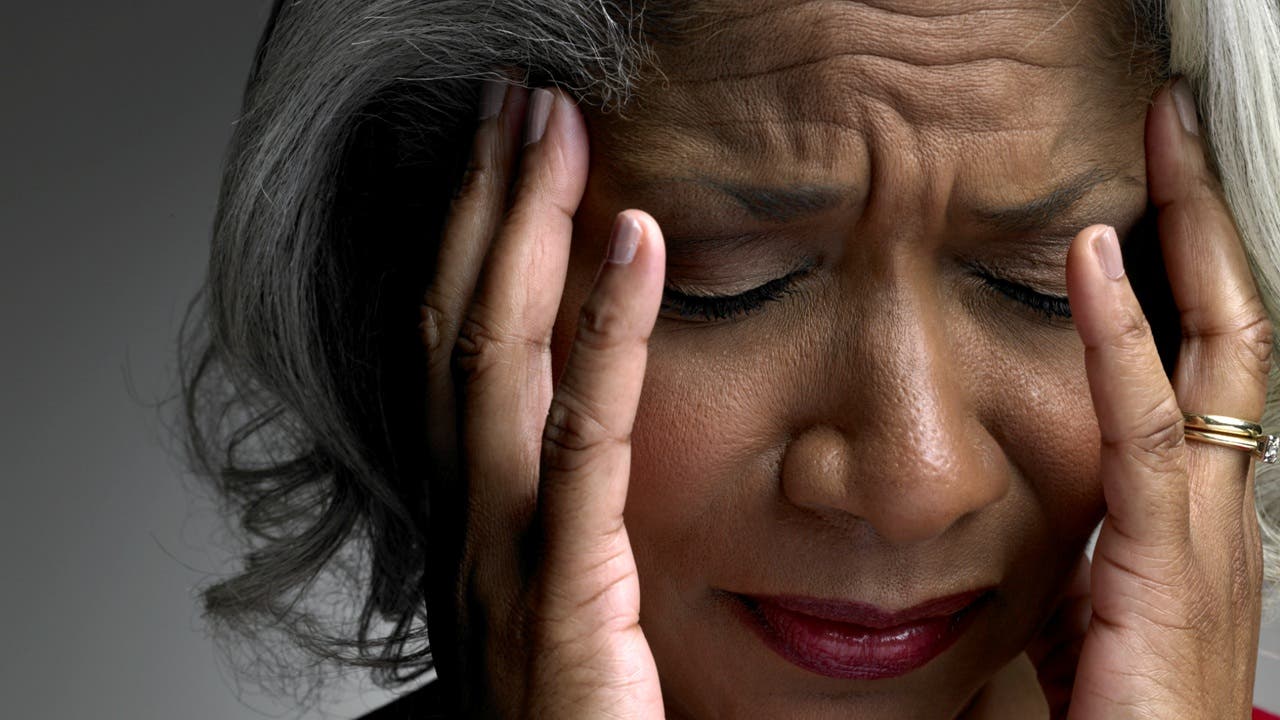
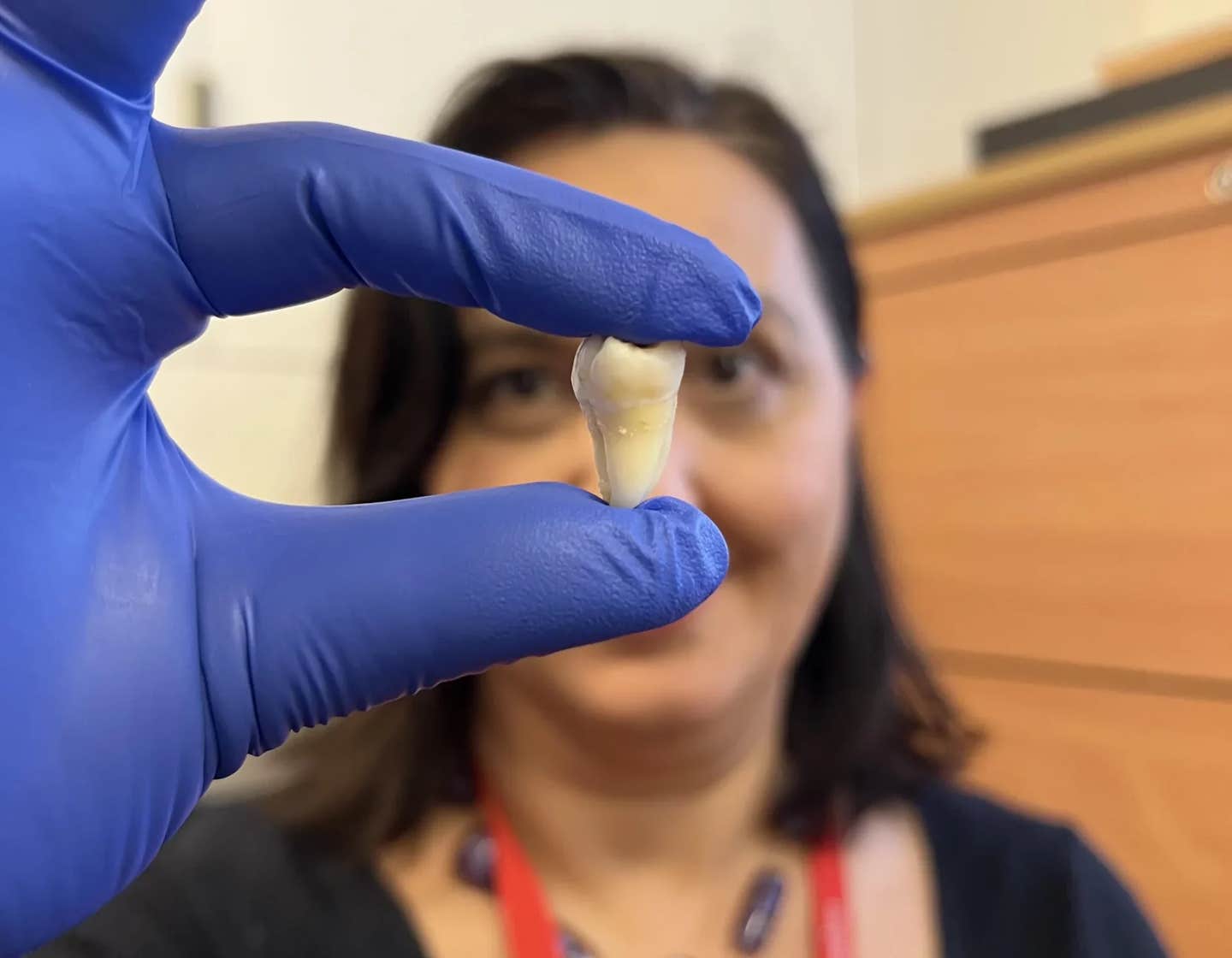
Migraine Headache (CREDIT: Johns Hopkins Medicine)
A migraine is far more than just a severe headache. It's part of a neurologic disorder with a variety of symptoms like pulsating head pain, nausea, vomiting, and sensitivity to light and sound. Migraines often strike without warning, causing significant disruption.
Adolescent girls with a family history of migraines are particularly susceptible, yet much about the disorder remains unknown. Dr. Hadas Nahman-Averbuch, a scientist at Washington University School of Medicine in St. Louis, is dedicated to uncovering these mysteries. She is spearheading two observational studies to investigate why some adolescent girls develop migraines and others do not, and to explore the role puberty plays in migraines for both boys and girls.
These studies, supported by $6 million in grants from the National Institutes of Health (NIH), are single-center studies at the School of Medicine.
“During adolescence, we see a significant increase in the prevalence of migraine diagnoses in girls,” said Nahman-Averbuch, an assistant professor of anesthesiology who runs the Pain Across the Lifespan lab. “We want to understand the changes that come before migraine headache onset and identify the girls who are at risk of developing them. The hope is that this knowledge leads to new therapies and interventions that, if given early, could prevent, manage, or treat migraine headaches in adolescent girls.
“We also want to investigate how puberty affects the severity and incidence of migraine headaches in adolescent girls and boys who already experience them, to better understand the trajectory of the disorder.”
Treatment options for young migraine sufferers are limited. Recent medications are typically available only to those 18 and older, highlighting the need for more research on this debilitating condition in adolescents.
Related Stories
Identifying the exact cause of migraines is challenging due to the many potential triggers, such as stress, certain foods, sleep deprivation, caffeine, and hormonal fluctuations. The inconsistent time delays between triggers and migraine onset further complicate this task.
In the first study, Nahman-Averbuch focuses on 200 girls aged 10 to 13. Participants undergo three visits where magnetic resonance imaging (MRI) examines brain connectivity between the amygdala and the prefrontal cortex. The amygdala plays a crucial role in pain perception and response, interacting with the prefrontal cortex. Changes in this interaction are noted in migraine patients and are linked to headache frequency in adolescents with the disorder.
Girls with a family history of migraines are compared to those without such history to see if brain changes can predict future diagnoses. These girls, migraine-free at the start, are monitored for two years to track migraine development.
Previous research indicates that adolescents with a first-degree relative with migraines have a higher sensitivity to pain. Nahman-Averbuch, involved in this earlier research, believes that a heightened response to sensory tests involving heat, cold, and pressure may predict future diagnoses. Participants rate these experiences as part of the study.
Migraine incidence is higher in boys before puberty and in girls during puberty, when sex hormones fluctuate significantly. Researchers aim to determine if specific hormones like estrogen, testosterone, or progesterone can predict why adolescent girls are more likely to be affected. The study includes monitoring blood levels of various sex hormones.
“There are many changes – biological, psychological, and social – happening during puberty,” Nahman-Averbuch said. “Each could impact the pain system and be responsible for this pattern. We want to figure out what those changes are, and if they can predict who is at risk of developing migraine headaches.”
The second study tracks 180 girls and boys aged 10 to 13 diagnosed with migraines over two years. Migraine-free boys with no family history and migraine-free girls from the first study serve as the control group. Using the same methods as the first study, researchers investigate how puberty impacts migraines.
“Understanding the changes that come before migraine headache onset and the changes during puberty that improve migraine disorder in a certain population can help us develop new interventions and preventive strategies,” Nahman-Averbuch said. “Meanwhile, identifying adolescents who are at risk may allow us to start such interventions earlier.”
These studies aim to shed light on the complexities of migraines and provide hope for better treatments and preventive measures for adolescents suffering from this challenging condition.
Typical causes of Migraine headaches in men and women
Migraines are complex and can be triggered by a variety of factors. The exact cause of migraines isn't fully understood, but it's believed to be related to a combination of genetic, environmental, and neurological factors. According to the Mayo Clinic, here are some common causes and triggers:
Genetic Factors
- Family History: Migraines often run in families, suggesting a genetic component.
- Genetic Mutations: Specific genetic mutations can affect brain function and susceptibility to migraines.
Neurological Factors
- Brain Chemistry: Changes in the brainstem and its interactions with the trigeminal nerve, a major pain pathway, are involved.
- Neurotransmitter Imbalances: Imbalances in brain chemicals, such as serotonin, which helps regulate pain, may play a role.
Environmental and Lifestyle Factors
- Hormonal Changes: Fluctuations in estrogen, particularly in women, can trigger migraines. This includes menstrual cycles, pregnancy, and menopause.
- Stress: Emotional stress and anxiety can trigger migraines.
- Sleep Patterns: Poor sleep or changes in sleep patterns can precipitate migraines.
Dietary Factors
- Certain Foods and Beverages: Aged cheeses, salty foods, processed foods, and food additives (such as aspartame and monosodium glutamate) are common triggers. Alcohol, especially wine, and caffeinated beverages can also trigger migraines.
- Skipping Meals: Irregular eating habits and fasting can lead to migraines.
Sensory Stimuli
- Bright Lights: Exposure to intense light or glare.
- Loud Noises: Prolonged exposure to loud sounds.
- Strong Smells: Perfumes, smoke, and other strong odors can initiate migraines.
Physical Factors
- Physical Exertion: Intense physical activity, including exercise and sexual activity, can trigger migraines.
- Changes in Weather: Variations in weather, particularly changes in barometric pressure, can be a trigger.
Medications
- Certain Medications: Some medications can provoke migraines, including oral contraceptives and vasodilators.
Other Health Conditions
- Other Health Conditions: Chronic conditions like depression, anxiety, and sleep disorders can contribute to the frequency and severity of migraines.
Managing migraines often involves identifying and avoiding personal triggers, maintaining a healthy lifestyle, and using medications as prescribed by a healthcare provider.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Joshua Shavit
Science & Technology Writer | AI and Robotics Reporter
Joshua Shavit is a Los Angeles-based science and technology writer with a passion for exploring the breakthroughs shaping the future. As a contributor to The Brighter Side of News, he focuses on positive and transformative advancements in AI, technology, physics, engineering, robotics and space science. Joshua is currently working towards a Bachelor of Science in Business Administration at the University of California, Berkeley. He combines his academic background with a talent for storytelling, making complex scientific discoveries engaging and accessible. His work highlights the innovators behind the ideas, bringing readers closer to the people driving progress.