Breakthrough protein could defeat Alzheimer’s disease and increase productive lifespan
Beyond its physiological toll, Alzheimer’s casts long shadows over individuals’ professional lives and eclipsing the joys of life’s twilight

[Oct. 20, 2023: Staff Writer, The Brighter Side of News]
Beyond its physiological toll, Alzheimer’s casts long shadows over individuals' professional lives and eclipsing the joys of life’s twilight. (CREDIT: Creative Commons)
Researchers at Temple University's Alzheimer's Center delve into the critical connections between ABCA7 protein, cholesterol metabolism, and inflammation, igniting hope for revolutionary treatments in Alzheimer's disease management.
Alzheimer’s disease, an enigmatic illness that insidiously disrupts memory, cognitive functions, and the very essence of self, has increasingly asserted its presence among the top causes of death worldwide.
Beyond its physiological toll, Alzheimer’s casts long shadows over individuals' professional lives, jolting financial stability, truncating careers, and eclipsing the joys of life’s twilight years. However, groundbreaking research is poised to redefine the landscape of this malady, potentially empowering patients with the autonomy to decide when to retire and ensuring an enhanced quality of life even as they age.
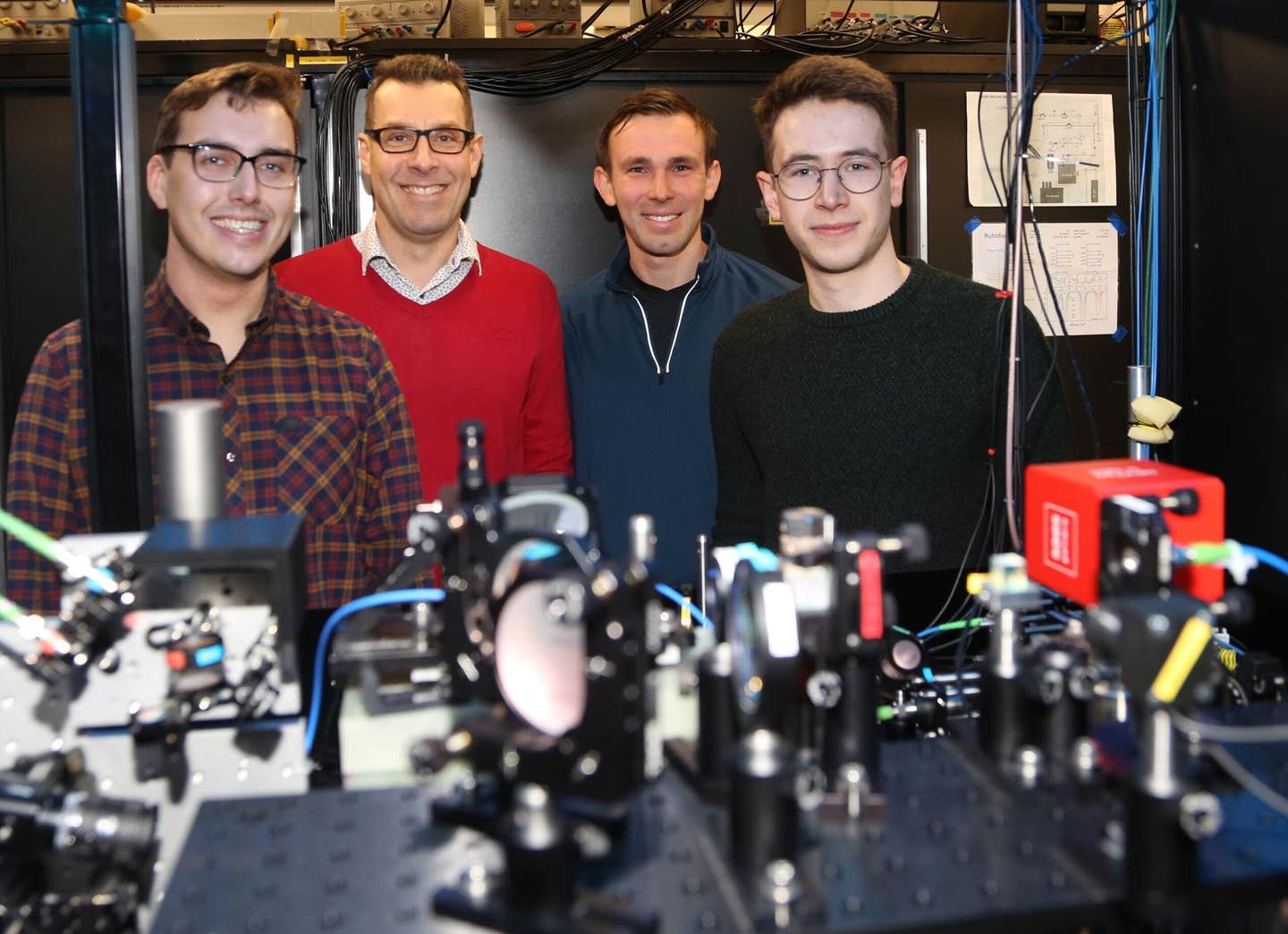
Heating causes a reduction in immunodetectable ABCA7 and ABCA1 in BHK-ABCA7 and BHK-ABCA1 cell lysate samples. (CREDIT: Cells)
At the forefront of this scientific crusade is the dedicated team at the Alzheimer’s Center at Temple, part of the esteemed Lewis Katz School of Medicine at Temple University. Their latest research, which was recently published in the acclaimed journal Cells, shines a spotlight on a protein called ABCA7. This protein, intriguingly linked with Alzheimer's protective mechanisms, could herald a new era in the effective treatment of this debilitating condition.
The journey to uncovering ABCA7's significance commenced with genome-wide association studies. These extensive, collaborative explorations of the human genome engaged thousands of participants, revealing the protein's potential role in Alzheimer's development.
ABCA7/Abca7 expression in cholesterol-depleted tissue in three publicly available RNA sequencing datasets. (CREDIT: Cells)
Joel Wiener, a key investigator with the Alzheimer’s Center at Temple and the pioneering author of this seminal study, explains, “While genome studies flag potential proteins of interest, they don’t decipher the functional mechanics or how these proteins influence disease progression. Our mission is not just to demystify ABCA7's functions but to harness this knowledge, transforming ABCA7 into a potent therapeutic ally against Alzheimer’s disease.”
This isn’t the first time the team at Temple has treaded the complex pathways linking ABCA7 and Alzheimer's. Prior research steered by Nicholas Lyssenko, Ph.D., a distinguished investigator at the Alzheimer’s Center at Temple and the principal author of the current study, unveiled that individuals aged between 63 and 78 with diminished levels of ABCA7 protein in their brains faced an elevated risk of succumbing to Alzheimer’s. This revelation not only supported earlier genome studies' deductions but also underscored ABCA7's protective armor for the human brain.
In their most recent endeavor, Dr. Lyssenko's cadre sought to unravel how cholesterol metabolism interplays with inflammation to orchestrate ABCA7 levels in human brain cells, thereby influencing the genesis of Alzheimer’s disease.
Related Stories
Their methodology was meticulously crafted, involving an array of experiments on diverse neural cell lines, including microglia, astrocytes, and neurons. Initially, they curtailed cholesterol levels in these cells, subsequently introducing them to rosuvastatin, a drug known for its cholesterol-inhibiting prowess.
To probe inflammation's impact on ABCA7, the scientists exposed the same cell varieties to major proinflammatory cytokines—specifically IL-1β, IL-6, or TNFα—which are notorious for inciting inflammation post secretion from certain immune cells.
The outcomes were revelatory. ABCA7 levels plummeted by approximately 40% in microglia cell lines and about 20% in an astrocyte cell line when these cells underwent a reduction of over half of their typical cholesterol content. Conversely, neuronal cell lines displayed an unaltered ABCA7 landscape post-cholesterol depletion.
Moreover, the cytokines IL-1β and TNFα curtailed ABCA7 expression singularly in microglial cells, while IL-6 remained ineffectual on ABCA7 in microglia. Astonishingly, none of the trio of cytokines induced any ABCA7 fluctuations in either astrocytes or neurons.
Mr. Wiener elaborated on the profound implications of their discoveries, “Our research indicates that cholesterol scarcity downregulates ABCA7 across various brain cells. This contrasts with previous mouse studies where cholesterol paucity actually elevated ABCA7.
Furthermore, while other studies identified inflammation's role in repressing ABCA7 in astrocytes, our findings illustrate a similar effect in microglia. Essentially, both diminished cholesterol and heightened inflammation could potentially dwindle ABCA7 levels in the brain, precipitating the onset of Alzheimer’s disease.”
The Temple collective’s investigative lens extends beyond human cells, encompassing experiments with animal models and postmortem human brain tissues. “The monumental hurdle we now face,” Dr. Lyssenko asserts, “is devising a methodology to accurately quantify ABCA7 levels in the brains of living individuals. Achieving this would not only confirm if inflammation indeed suppresses ABCA7 in humans but also pave the way for identifying those at heightened Alzheimer's risk, thereby catalyzing the creation of innovative ABCA7-centric therapies.”
The study's contributors, a blend of distinguished and emerging researchers—including Sindy Desire, Viktor Garliyev, Nicholas Lyssenko III, and Domenico Praticò—belong to the Alzheimer's Center at Temple, Department of Neural Sciences, Lewis Katz School of Medicine.
Their collective endeavor marks a significant stride towards illuminating the mysteries shrouding Alzheimer’s and, more importantly, offers a beacon of hope for millions grappling with the disease, their families, and caregivers worldwide.
Who has Alzheimer’s Disease?
In 2020, as many as 5.8 million Americans were living with Alzheimer’s disease.
Younger people may get Alzheimer’s disease, but it is less common.
The number of people living with the disease doubles every 5 years beyond age 65.
This number is projected to nearly triple to 14 million people by 2060.
Symptoms of the disease can first appear after age 60, and the risk increases with age.
What is known about Alzheimer’s Disease?
Scientists do not yet fully understand what causes Alzheimer’s disease. There likely is not a single cause but rather several factors that can affect each person differently.
Age is the best known risk factor for Alzheimer’s disease.
Family history—researchers believe that genetics may play a role in developing Alzheimer’s disease. However, genes do not equal destiny. A healthy lifestyle may help reduce your risk of developing Alzheimer’s disease. Two large, long term studies indicate that adequate physical activity, a nutritious diet, limited alcohol consumption, and not smoking may help people.
Changes in the brain can begin years before the first symptoms appear.
Researchers are studying whether education, diet, and environment play a role in developing Alzheimer’s disease.
There is growing scientific evidence that healthy behaviors, which have been shown to prevent cancer, diabetes, and heart disease, may also reduce risk for subjective cognitive decline.
What is the burden of Alzheimer’s disease in the United States?
Alzheimer’s disease is one of the top 10 leading causes of death in the United States.
The 6th leading cause of death among US adults.
The 5th leading cause of death among adults aged 65 years or older.
In 2020, an estimated 5.8 million Americans aged 65 years or older had Alzheimer’s disease. This number is projected to nearly triple to 14 million people by 2060.
In 2010, the costs of treating Alzheimer’s disease were projected to fall between $159 and $215 billion. By 2040, these costs are projected to jump to between $379 and more than $500 billion annually.
Death rates for Alzheimer’s disease are increasing, unlike heart disease and cancer death rates that are on the decline.
Dementia, including Alzheimer’s disease, has been shown to be under-reported in death certificates and therefore the proportion of older people who die from Alzheimer’s may be considerably higher.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get the Brighter Side of News' newsletter.
Joseph Shavit
Head Science News Writer | Communicating Innovation & Discovery
Based in Los Angeles, Joseph Shavit is an accomplished science journalist, head science news writer and co-founder at The Brighter Side of News, where he translates cutting-edge discoveries into compelling stories for a broad audience. With a strong background spanning science, business, product management, media leadership, and entrepreneurship, Joseph brings a unique perspective to science communication. His expertise allows him to uncover the intersection of technological advancements and market potential, shedding light on how groundbreaking research evolves into transformative products and industries.