Breakthrough new treatment could stop cancer from reaching the brain
Researchers identify a critical vulnerability in brain metastases, opening the door to therapies targeting cancer spread before it takes hold.

A new study uncovers vulnerabilities in brain metastases, offering hope for therapies that target cancer spread and improve survival outcomes. (CREDIT: iStock)
Brain metastases (BMs) are a devastating complication of cancer, occurring ten times more frequently than primary brain tumors. Patients diagnosed with BMs face grim survival odds, with a 90% mortality rate within 4 to 12 months of diagnosis.
Lung cancer, breast cancer, and melanoma are the primary cancers responsible for 85% of these cases. While advances in treating primary cancers have prolonged patient lives, they have also increased the incidence of brain metastases. Current treatments, such as surgery and radiation, are palliative and rarely curative, underscoring the urgency for new therapeutic strategies.
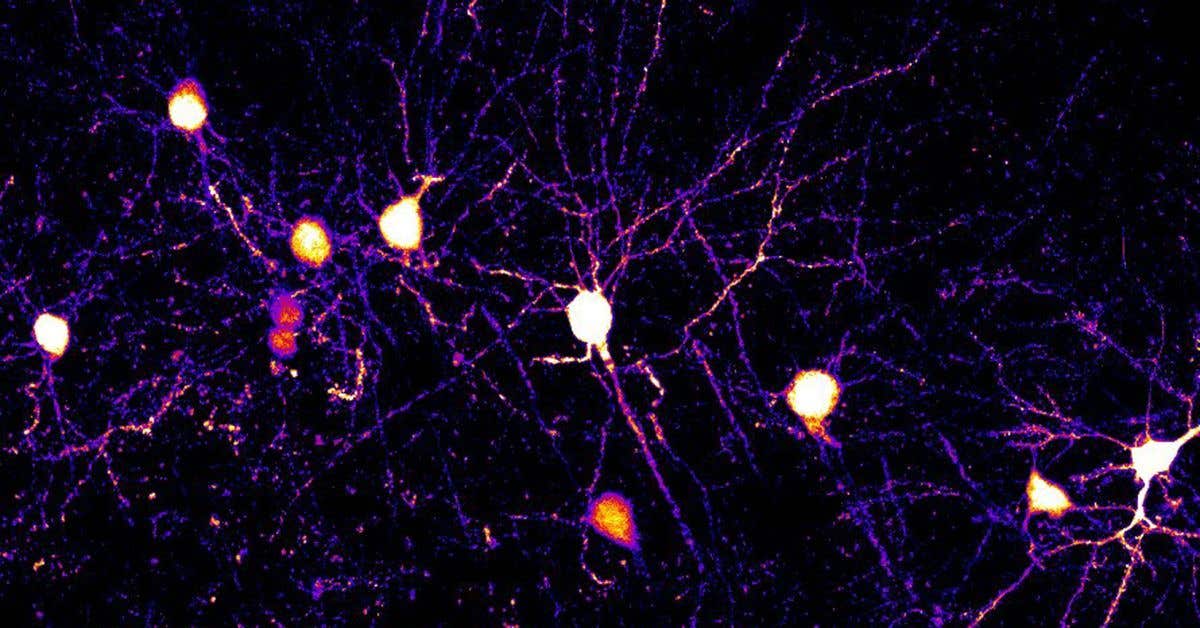
Primary tumors contain diverse cell populations, each with varying capacities for proliferation, differentiation, and metastasis.
Only an estimated 0.01% of cancer cells possess the ability to initiate secondary tumors. These specialized cells, referred to as brain metastasis-initiating cells (BMICs), exhibit stem-like qualities that drive tumor growth and contribute to therapy resistance and relapse.
BMICs can evade conventional treatments and migrate from their primary tumor to the brain, establishing metastatic colonies. Researchers believe that targeting BMICs before they fully colonize the brain could be a game-changer.
Sheila Singh, a professor at McMaster University, explains, “We’re getting much better at curing primary cancers, but even when we do, a tiny percentage of cancer cells can escape and circulate to other parts of the body, including the brain. When this happens, it’s often an end-stage cancer — treatment-resistant and highly evasive.”
Singh and her colleagues recently identified a critical vulnerability in BMICs: an enzyme called inosine monophosphate dehydrogenase (IMPDH). This enzyme plays a key role in the metabolic pathway of guanosine triphosphate (GTP) synthesis, essential for BMIC survival and proliferation. By targeting this pathway, researchers aim to prevent cancer cells from metastasizing to the brain.
The McMaster University team utilized advanced computational tools like Connectivity Map analysis to examine the genetic profiles of BMICs derived from lung, breast, and melanoma cancers.
This analysis, published in the journal, Cell Reports Medicine, revealed that purine metabolism is a metabolic vulnerability in BMICs. Mycophenolic acid (MPA), an existing IMPDH inhibitor, emerged as a potential therapeutic agent. However, its limited ability to cross the blood-brain barrier necessitated further innovation.
Related Stories
To overcome this hurdle, the researchers synthesized a library of MPA analogs designed for better brain penetration. Among these, one compound, known as Compound 3, demonstrated superior efficacy in animal models, significantly extending survival times. Mechanistic studies confirmed that inhibiting IMPDH effectively reduced BMIC activity and delayed the formation of brain metastases.
Jakob Magolan, a professor of medicinal chemistry at McMaster, likens BMICs to ships leaving a harbor, representing their journey from the primary tumor to the brain. “We have figured out how to sink these ships while they’re in transit — and likely before they even set sail,” he says. By disrupting BMIC’s metabolic machinery, the researchers hope to prevent metastatic spread at its earliest stages.
The scale and ambition of this research are noteworthy, involving the synthesis and evaluation of over 500 candidate molecules. Typically, pharmaceutical companies would create about 1,000 molecules in a drug discovery program.
Achieving this milestone in an academic setting highlights the dedication of the interdisciplinary team, which includes staff, students, and trainees.
One such trainee, Agata Kieliszek, a postdoctoral fellow and lead author of the study, expresses optimism about the potential impact of their findings. “Brain metastases are the most common brain tumors in adults, and the standard of care is largely palliative,” she explains. “With this work, we’ve uncovered a target for slowing brain metastasis outgrowth, which, with further research, could offer an alternative treatment option for patients who are otherwise limited to palliation.”
The study has received substantial support, including $2 million in funding from adMare BioInnovations. This collaboration has driven rapid progress in optimizing lead compounds for pre-clinical evaluation. “We’re more than halfway through an industrial-sized program now, with promising compounds in hand,” Magolan notes.
The team’s progress positions them for eventual clinical trials, which could pave the way for a new standard of care in preventing brain metastases.
While this research focuses on brain metastases, its implications extend to other forms of metastatic cancer. The principles underlying metastasis to the brain may also apply to the spread of cancer to other organs.
Magolan shares his hopes for the broader impact of their work, saying, “The compounds that we’re looking at prevent spread to the brain, but the principles of metastasis are potentially similar across other organs. I am hopeful that this program might open a gateway to anti-metastasis therapies that can prevent other types of cancer spread.”
The team plans to spin out a start-up company dedicated to translating these findings into a precision medicine approach. With dozens of potent compounds identified and promising results from animal studies, the researchers are optimistic about the future. Their work not only offers hope for patients with brain metastases but also lays the groundwork for a paradigm shift in cancer treatment.
Adding to the broader significance of this research, experts suggest that the compounds under investigation could inspire new treatments for metastases in organs such as the liver or lungs. By refining the molecules to specifically inhibit BMIC function across different cancer types, the researchers aim to address one of oncology’s greatest challenges.
Furthermore, ongoing studies are focusing on understanding the precise mechanisms that enable BMICs to resist conventional therapies, providing additional opportunities for targeted interventions.
As the team moves toward clinical trials, they remain committed to collaborative efforts with pharmaceutical partners and academic institutions. This partnership model not only accelerates the path to new therapies but also ensures that the research benefits a wide range of patients.
With their eyes set on the horizon, the researchers’ groundbreaking work holds the promise of transforming how metastatic cancer is treated worldwide.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Joseph Shavit
Head Science News Writer | Communicating Innovation & Discovery
Based in Los Angeles, Joseph Shavit is an accomplished science journalist, head science news writer and co-founder at The Brighter Side of News, where he translates cutting-edge discoveries into compelling stories for a broad audience. With a strong background spanning science, business, product management, media leadership, and entrepreneurship, Joseph brings a unique perspective to science communication. His expertise allows him to uncover the intersection of technological advancements and market potential, shedding light on how groundbreaking research evolves into transformative products and industries.