Breakthrough implantable sensors enable real-time inflammation monitoring
Implantable sensors are revolutionizing healthcare by enabling real-time protein monitoring for inflammation and chronic diseases.
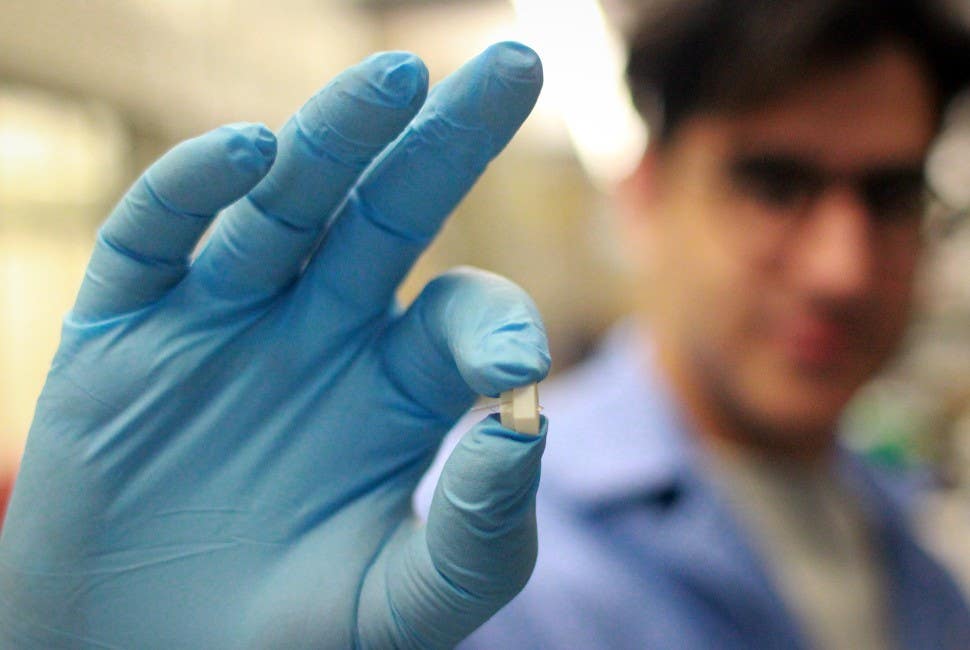
Postdoctoral fellow Hossein Zargartalebi, the study’s first author, holds the first-of-its-kind sensor, which monitors fluctuating proteins within the body in real time. (CREDIT: Northwestern University)
Continuous monitoring of protein biomarkers in the body has been a significant scientific challenge, yet it holds transformative potential for managing and preventing diseases. Current wearable and implantable sensors excel at tracking small molecules like glucose and electrolytes.
However, when it comes to proteins—key indicators of inflammation and other health conditions—the field has lagged. Proteins present in low concentrations and with slow binding dynamics have been difficult to measure in real time. A breakthrough now promises to overcome these barriers.
A team of researchers at Chan Zuckerberg Biohub Chicago and Northwestern University recently unveiled an innovative implantable sensor capable of continuously tracking protein fluctuations in living organisms. The proof-of-concept study, published in Science, demonstrated how this technology monitored inflammation markers in diabetic rats with unprecedented sensitivity and accuracy.
This milestone technology, likened to a "continuous glucose monitor for proteins," enables real-time tracking of inflammation—a biological process implicated in diseases responsible for half of all global deaths, including heart disease and cancer.
"This is a completely new capability—to be able to watch inflammation in real time," remarked Shana Kelley, a senior researcher on the project and president of CZ Biohub Chicago.
The Challenge of Monitoring Proteins in Real Time
Proteins play vital roles in cellular communication and immune response, with their levels serving as critical health indicators. However, traditional sensors struggle with the strong and prolonged binding of proteins to detection molecules, making it nearly impossible to measure dynamic changes.
For example, sensors using high-affinity receptors like antibodies experience binding half-lives of up to 20 hours, rendering them unsuitable for real-time applications.
Related Stories
Current diagnostic tools rely on blood or urine tests, which provide only snapshots of protein levels. While these methods have been essential for understanding health trends, they fail to capture the rapid fluctuations crucial in conditions like inflammation, diabetes, or heart failure. Continuous monitoring of proteins in vivo could fill this critical gap.
The breakthrough lies in a novel approach inspired by simple natural processes. Lead researcher Hossein Zargartalebi compared the mechanism to shaking apples off a tree. The sensor uses nanoscale DNA-based receptors attached to electrodes.
When an alternating electric field is applied, the DNA strands oscillate like pendulums, shaking off bound proteins within seconds and resetting for the next measurement. This active-reset mechanism enables the sensor to provide real-time feedback on protein concentration changes.
"We recognized this fundamental obstacle and developed the idea that maybe we can shake the proteins right off the sensors," Kelley explained. "The first time we tried it, it worked beautifully."
Testing in Diabetic Rats
The researchers designed an implantable device containing the sensors within a microneedle, comparable in size to those used in continuous glucose monitors. This microneedle, thinner than three human hairs, samples interstitial fluid just beneath the skin. The device was tested on diabetic rats, a model system where inflammation plays a significant role in disease complications.
The sensors monitored two cytokines, key protein markers of inflammation. When the rats fasted or received insulin, cytokine levels decreased, reflecting reduced inflammation. Conversely, injections of immune-activating substances caused cytokine levels to spike. These measurements closely matched gold-standard laboratory methods, affirming the device's accuracy.
Even subtle inflammation, such as that caused by the needle itself during insulin injections, was detected by the sensors. This exceptional sensitivity underscores the technology's potential for tracking minute biological changes.
The implications of this technology extend beyond inflammation monitoring. Kelley envisions its application in managing other conditions where proteins are critical biomarkers.
For instance, in heart failure, tracking levels of B-type natriuretic peptide (BNP) in real time could enable earlier interventions. Currently, BNP levels are typically checked during quarterly doctor visits, leaving gaps in monitoring that could delay treatment.
"If you have heart failure, you might go to the doctor every three months," Kelley noted. "But symptoms often occur between visits. With a continuous monitor, doctors could access real-time data and adjust medications before symptoms worsen."
The device also has potential applications in understanding immune system behavior. The team aims to use it in tissue models embedded with thousands of sensors, exploring how immune cells behave in real time and identifying critical tipping points that lead to disease.
Toward Human Applications
While the current study focused on rats, researchers are optimistic about adapting the technology for humans. By making continuous protein monitoring feasible, this innovation could revolutionize how chronic and acute diseases are managed.
The ability to monitor inflammation and other biomarkers in real time could lead to earlier diagnoses, more personalized treatments, and even preventive strategies.
"This has the same potential to allow us to monitor, and even prevent, many diseases," Kelley said. "With inflammation, the sky’s the limit with what you could do for your health by keeping a handle on it."
The collaborative efforts of scientists, engineers, and physicians at CZ Biohub Chicago exemplify how interdisciplinary research can yield groundbreaking solutions. Funded by the Chan Zuckerberg Initiative and other prominent institutions, this work underscores the transformative power of innovation in healthcare.
This active-reset sensor represents a critical leap forward in bioelectronic technology, setting the stage for real-time health monitoring on a molecular scale. As researchers refine the device and explore additional applications, the potential benefits for human health are vast.
From managing inflammation to monitoring heart failure and beyond, this technology could become a cornerstone of preventive medicine.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Rebecca Shavit
Science & Technology Journalist | Innovation Storyteller
Based in Los Angeles, Rebecca Shavit is a dedicated science and technology journalist who writes for The Brighter Side of News, an online publication committed to highlighting positive and transformative stories from around the world. With a passion for uncovering groundbreaking discoveries and innovations, she brings to light the scientific advancements shaping a better future. Her reporting spans a wide range of topics, from cutting-edge medical breakthroughs and artificial intelligence to green technology and space exploration. With a keen ability to translate complex concepts into engaging and accessible stories, she makes science and innovation relatable to a broad audience.



