Breakthrough immunotherapy drug revolutionizes pancreatic cancer treatment
Breakthrough research on NKT cells and folinic acid offers hope for improved immunotherapy against pancreatic cancer’s defenses.
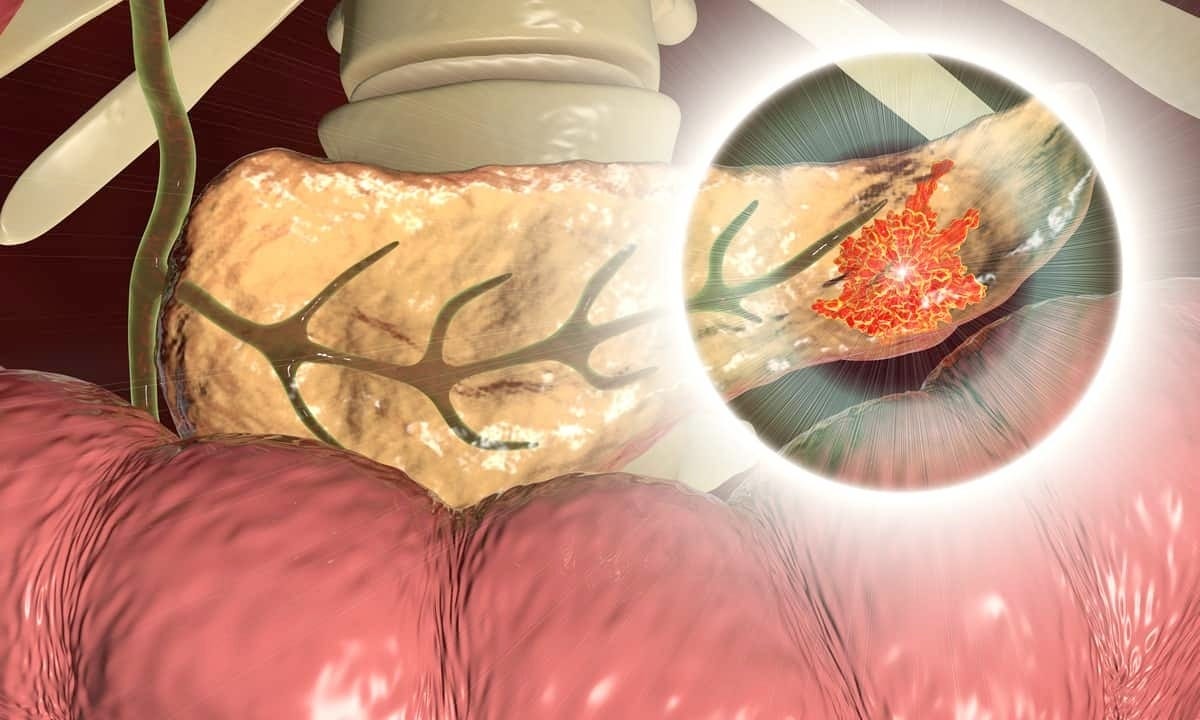
Scientists discover how NKT cells and folinic acid break pancreatic cancer’s defenses. (CREDIT: CC BY-SA 4.0)
Pancreatic ductal adenocarcinoma (PDAC) is among the deadliest cancers, with a survival rate of just 11%. A primary culprit behind this grim statistic is its immunosuppressive tumor microenvironment (TME), which blocks immune cells from effectively targeting tumors.
Traditional treatments struggle against this cancer’s resilient defenses, leaving many patients with limited options. Yet, recent breakthroughs in understanding PDAC's immune dynamics are sparking hope for new therapies.
Immunotherapy, particularly immune checkpoint blockade, has revolutionized cancer treatment. By targeting proteins like PD-1 and CTLA-4, these therapies unleash the immune system’s natural ability to fight cancer.
However, PDAC remains largely resistant, with fewer than 5% of cases responding to checkpoint inhibitors. This resistance stems from an immunologically “cold” TME, where cancer-fighting T cells struggle to penetrate the tumor and immunosuppressive cells dominate.
“Immune checkpoint therapy is only an option in rare cases of PDAC,” says Cold Spring Harbor Laboratory (CSHL) Professor Douglas Fearon. “It’s only effective for patients with a specific subtype of PDAC—that’s less than 5% of all cases.”
NKT Cells and Type-I Interferons
Contrary to earlier assumptions that PDAC evades any immune detection, recent findings reveal that immune cells do attempt to fight the cancer but are blocked by its robust defenses. Natural killer T (NKT) cells, a rare subset of immune cells, play a pivotal role in overcoming these barriers.
These cells, known for their ability to bridge innate and adaptive immunity, produce cytokines and interact with other immune cells to amplify antitumor responses.
Related Stories
Key to this process is type-I interferon (IFN), a signaling molecule essential for a robust antitumor immune response. NKT cells facilitate the production of type-I IFN through CD40-CD40L interactions with myeloid cells. This signaling cascade not only recruits other immune cells, such as T cells and dendritic cells, into the tumor but also primes them for action.
“We discovered that NKT cells enabled type-I interferon to be produced and, as a consequence, adaptive immune killing and expansion of T cells would occur,” says Fearon.
Folinic Acid: Cracking PDAC’s Defenses
Fearon’s team, in collaboration with former postdoctoral researcher Jiayun Li, recently uncovered a surprising ally in the fight against PDAC: folinic acid. This common chemotherapy supplement boosts levels of NKT cells and type-I IFN within PDAC tumors in mice, breaking through the cancer’s defenses.
By disrupting PDAC’s protective shield, formed by the proteins CXCR4 and CXCL12, folinic acid allows immune cells to infiltrate and attack the tumor.
“Folinic acid enhances that response,” explains Fearon. “T cells respond to tumors, but they typically cannot get in there unless type-I interferon is produced.”
When administered to mice with PDAC, folinic acid slows tumor growth and extends survival. It also improves the effectiveness of anti-PD-1 therapies, which are otherwise ineffective in most PDAC cases. This combination treatment demonstrates the potential to transform immunotherapy outcomes for PDAC patients.
Bridging the Gap Between Mice and Humans
While these findings are promising, translating them into human therapies remains a challenge. To address this, Fearon’s lab has partnered with Autobahn Labs, a biotech firm, to develop drugs targeting CXCR4 and CXCL12. These drugs aim to replicate folinic acid’s effects, making immune checkpoint therapy a viable option for a broader range of PDAC patients.
“Translating observations in mice into human therapy has been difficult,” Fearon acknowledges. “But if we’re successful, immunotherapy may one day become a viable choice for all patients with PDAC—and every other solid tumor—not just in the rare cases we see today.”
The insights gained from this research extend beyond PDAC. Understanding how NKT cells and type-I IFN orchestrate antitumor immunity could inform treatments for other immunologically “cold” tumors.
By targeting the molecular mechanisms that suppress immune responses, scientists are paving the way for therapies that activate the body’s natural defenses against even the most resilient cancers.
While much work remains, these discoveries mark a significant step toward dismantling PDAC’s defenses. For patients, this research represents a glimmer of hope in the fight against a formidable adversary.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Joshua Shavit
Science & Technology Writer | AI and Robotics Reporter
Joshua Shavit is a Los Angeles-based science and technology writer with a passion for exploring the breakthroughs shaping the future. As a contributor to The Brighter Side of News, he focuses on positive and transformative advancements in AI, technology, physics, engineering, robotics and space science. Joshua is currently working towards a Bachelor of Science in Business Administration at the University of California, Berkeley. He combines his academic background with a talent for storytelling, making complex scientific discoveries engaging and accessible. His work highlights the innovators behind the ideas, bringing readers closer to the people driving progress.



