Breakthrough drug reverses groin hernias without surgery
Scientists successfully reversed inguinal hernias in mice using medication, offering hope for a nonsurgical treatment in humans.

A groundbreaking study has identified estrogen receptor-alpha as a key driver of inguinal hernias and successfully reversed the condition. (CREDIT: CC BY-SA 4.0)
Inguinal hernias affect millions of men, with half of them likely to develop the condition by age 75. These hernias occur when soft tissue protrudes through weak abdominal muscles in the groin. Despite their prevalence, the biological mechanisms behind them remain largely unknown.
Treatment has historically relied on surgery, which comes with complications, particularly for older individuals. Even after surgical intervention, hernias return in 10-15% of cases, underscoring the need for alternative treatments.
A recent breakthrough from Northwestern Medicine challenges the notion that surgery is the only option. Researchers successfully reversed hernias in male mice using medication, offering hope for a nonsurgical treatment in humans.
Their study, published in the Journal of Clinical Investigation, also identified a key molecular factor: estrogen receptor-alpha (ESR1). This receptor appears to drive the excessive connective tissue buildup responsible for hernia formation. Importantly, human hernia tissue exhibited the same molecular markers as the mouse models, suggesting that men might respond to the treatment in the same way.
Understanding the Biology of Hernias
Inguinal hernias stem from muscle weakness in the lower abdomen, yet the exact biological triggers remain unclear. To investigate, researchers used a genetically modified mouse model known as Aromhum 11.
These mice express the human aromatase gene, mimicking the way testosterone converts to estrogen in aging men. This increase in estrogen triggers changes in skeletal muscle fibroblasts—connective tissue cells—leading to fibrosis and hernia development.
Single-cell RNA sequencing revealed a distinct cluster of fibroblasts in the weakened muscle known as hernia-associated fibroblasts (HAFs). These cells exhibit high ESR1 expression and show characteristics of pathological fibroblasts, including excessive proliferation and extracellular matrix remodeling.
Related Stories
HAFs also express markers of fibro-adipogenic progenitors (FAPs), a type of muscle-resident stem cell involved in tissue repair. When dysregulated, FAPs contribute to excessive scar tissue, mirroring what occurs in diseases like muscular dystrophy.
In Aromhum mice, the activation of ESR1 in fibroblasts appears to be a major driver of hernia formation. This suggests that blocking ESR1 could prevent or even reverse the condition.
A Drug-Based Approach to Hernia Repair
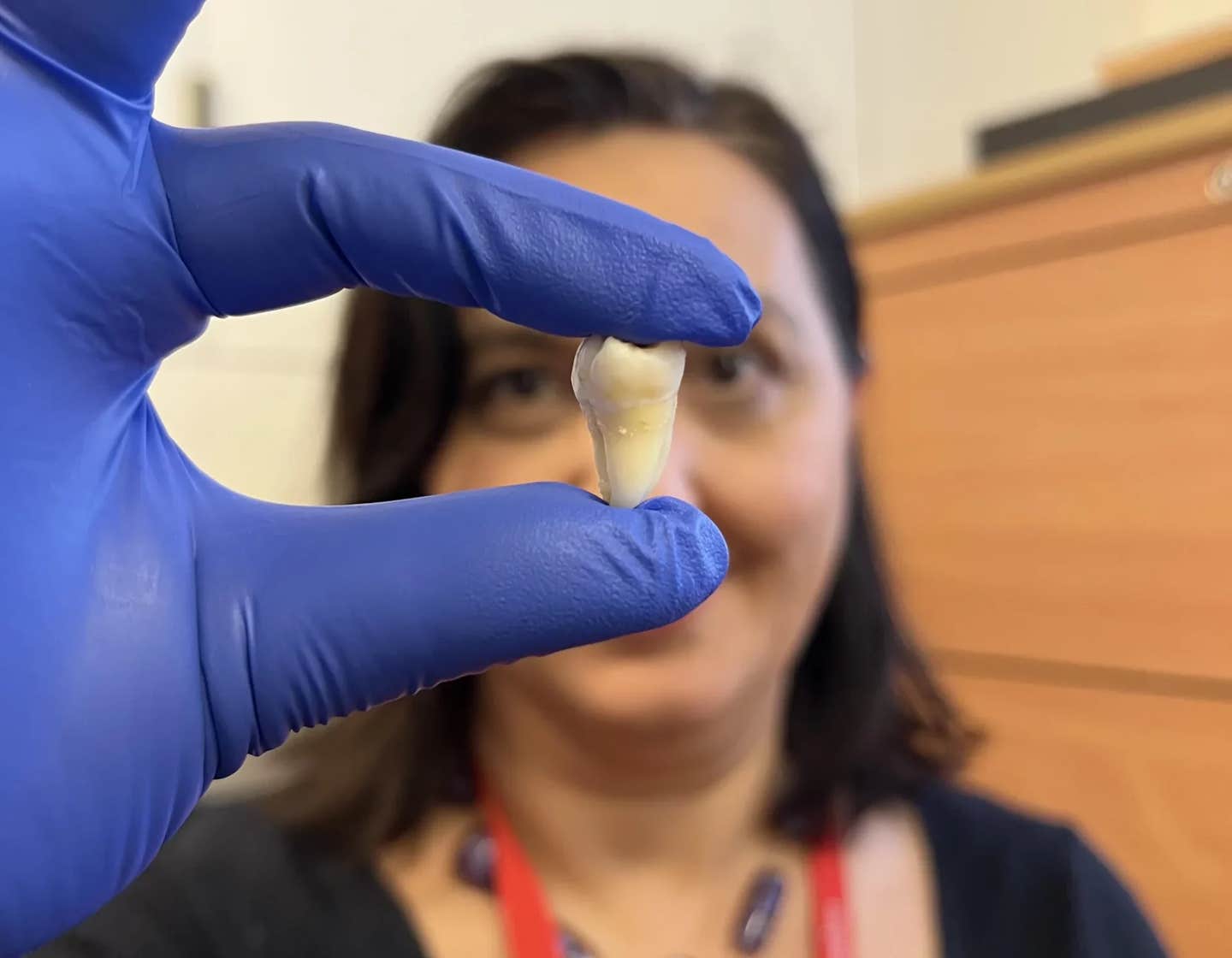
The research team tested this hypothesis using the drug fulvestrant, an estrogen receptor blocker already approved for treating certain types of breast cancer. The study involved two experimental arms—one using the mouse model and the other examining human hernia tissue.
In the mouse experiment, scientists injected fulvestrant to block ESR1 activity. The results were striking. Large hernias shrank, and the muscle structure returned to a healthy state. This demonstrated that targeting ESR1 could not only prevent but also reverse hernias.
To validate these findings in humans, researchers biopsied tissue samples from hernia patients, comparing affected areas to adjacent healthy muscle. They found identical molecular markers, confirming that ESR1-driven fibrosis plays a key role in both mice and humans.
Further analysis showed that estrogen and ESR1 activate gene networks linked to excessive scarring—providing direct evidence that estrogen signaling contributes to hernia development.
“We expect that estrogen/ESR1 is a promising molecular target for developing pharmaceutical treatments for inguinal hernia in men,” said Dr. Hong Zhao, a research professor at Northwestern University Feinberg School of Medicine.
Implications for Nonsurgical Treatment
The implications of this discovery could be significant, particularly for older patients or those with high surgical risks. Each year, more than one million inguinal hernia surgeries are performed in the U.S., many under general anesthesia. However, surgery does not address the underlying muscle weakness, which may explain the high recurrence rate in elderly men.
“This is a blockbuster publication about the first medical treatment of inguinal hernias,” said Dr. Serdar Bulun, chair of obstetrics and gynecology at Northwestern. “Our findings strongly suggest that men would also respond to this medication as the male mice did, so if male patients are high risk for surgery, we can one day try to repair the hernias medically.”
While inguinal hernias are less common in women—affecting one woman for every 34 men—they can still be problematic. In severe cases, hernias can lead to life-threatening complications such as bowel strangulation. A medical therapy could prevent these outcomes, improving patient care and reducing the need for invasive procedures.
The Future of Hernia Research
Although fulvestrant proved effective in mice, clinical trials will be necessary to determine its safety and efficacy in humans. Researchers also plan to explore other drugs that target ESR1, potentially developing more tailored therapies for hernia prevention and treatment.
The discovery of ESR1’s role in hernia formation marks a major step forward in understanding this common yet poorly understood condition. By shifting focus from surgical repair to biological intervention, scientists may pave the way for a new era in hernia treatment—one that could eliminate the need for invasive procedures and improve outcomes for millions of patients worldwide.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Rebecca Shavit
Science & Technology Journalist | Innovation Storyteller
Based in Los Angeles, Rebecca Shavit is a dedicated science and technology journalist who writes for The Brighter Side of News, an online publication committed to highlighting positive and transformative stories from around the world. With a passion for uncovering groundbreaking discoveries and innovations, she brings to light the scientific advancements shaping a better future. Her reporting spans a wide range of topics, from cutting-edge medical breakthroughs and artificial intelligence to green technology and space exploration. With a keen ability to translate complex concepts into engaging and accessible stories, she makes science and innovation relatable to a broad audience.