Breakthrough discovery could stop cold sores before they start
Until now, scientists believed that the herpes simplex virus simply waited for external triggers like stress or illness.

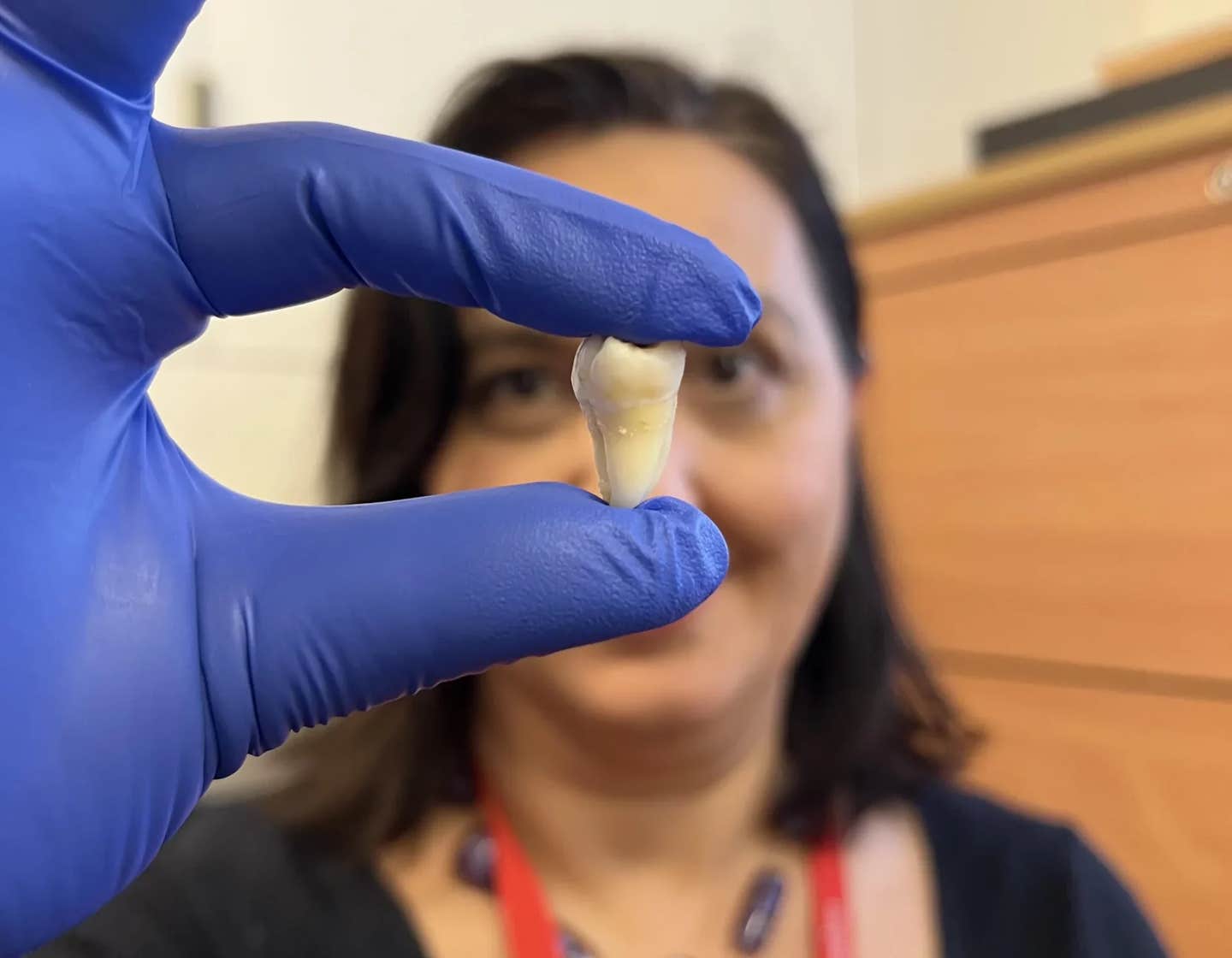
New research uncovers how the herpes virus hijacks immune pathways to trigger its reactivation. (CREDIT: CC BY-SA 4.0)
Scientists have uncovered a surprising trick used by the herpes simplex virus to wake up inside the body. Researchers at the University of Virginia School of Medicine have found that a viral protein, called UL12.5, plays a key role in this reactivation. This finding shakes up the traditional view of how the virus escapes its dormant state.
The discovery could lead to better treatments for cold sores and genital herpes, two conditions caused by the herpes simplex virus (HSV-1). Until now, scientists believed that the virus simply waited for external triggers like stress or illness. This new work shows that HSV-1 is much more active in its own revival.
Herpes: A Persistent Pathogen
HSV-1 is a highly contagious virus that infects more than 60% of people under 50, according to the World Health Organization. After the initial infection, the virus hides inside nerve cells for life. It can reactivate during times of stress, sickness, or even after sun exposure, causing symptoms to flare up again.
Most people know HSV-1 for causing cold sores. However, it can also lead to genital herpes and serious conditions like encephalitis. Studies have even linked it to neurodegenerative diseases, including Alzheimer's disease, making this research even more urgent.
When HSV-1 first invades a cell, the immune system’s pattern recognition receptors (PRRs) sound the alarm. These receptors spot pieces of the virus and trigger a defense response meant to wipe out the invader. Yet, like many viruses, HSV-1 has evolved sneaky ways to dodge or even control these defenses.
UL12.5 and Viral Reactivation
In a twist that surprised researchers, HSV-1 doesn’t just hide and wait for the right moment to reactivate. Instead, it helps create the right conditions itself. Scientists at UVA, led by Anna Cliffe, Ph.D., discovered that the virus expresses the protein UL12.5, which tricks the immune system into helping the virus wake up.
UL12.5 stimulates the immune system in a way that, paradoxically, promotes viral reactivation rather than fighting it. This clever move shows how viruses can turn the body’s defenses to their own advantage. It opens up exciting new paths for research into how we might block HSV-1 reactivation in the future.
Related Stories
UL12.5 targets mitochondria, the cell’s energy-producing structures, causing them to release mitochondrial DNA (mtDNA) into the cytosol. This triggers the cGAS-STING pathway, a major immune response mechanism that typically fights infections.
Under normal circumstances, cGAS detects foreign DNA in the cytosol and activates STING, which initiates the production of interferons and other antiviral molecules.
However, HSV-1 exploits this pathway to reawaken from dormancy. By inducing mitochondrial stress and the release of mtDNA, UL12.5 sets off a chain reaction that promotes viral gene expression and reactivation.
“We were surprised to find that HSV-1 doesn’t just passively wait for the right conditions to reactivate – it actively senses danger and takes control of the process,” said researcher Patryk Krakowiak. “Our findings suggest that the virus may be using immune signals as a way to detect cellular stress—whether from neuron damage, infections, or other threats—as a cue to escape its host and find a new one.”
Implications for Treatment and Prevention
Understanding how HSV-1 manipulates the immune system opens the door to new therapeutic strategies. Current antiviral drugs, such as acyclovir, only suppress viral replication during active infection but cannot prevent reactivation. The discovery of UL12.5’s role in awakening the virus suggests that targeting this protein could prevent outbreaks.
“We are now following up on this work to investigate how the virus is hijacking this response and testing inhibitors of UL12.5 function,” Cliffe said. “Currently, there are no therapies that can prevent the virus from waking up from dormancy, and this stage was thought to only use host proteins. Developing therapies that specifically act on a viral protein is an attractive approach that will likely have fewer side effects than targeting a host protein.”
The study also found that in cases where another infection was present, HSV-1 did not require UL12.5 for reactivation. Instead, the immune response triggered by the second infection was sufficient to wake up the virus. This suggests that HSV-1 can use multiple pathways to reactivate, further complicating treatment strategies.
The Connection to Neurodegenerative Disease
Beyond cold sores and genital herpes, HSV-1 has been linked to serious neurological conditions. Some research suggests that chronic inflammation from repeated HSV-1 reactivation may contribute to diseases such as Alzheimer’s. The ability of HSV-1 to manipulate immune pathways in neurons raises concerns about its long-term effects on brain health.
The virus establishes latency in neurons, where it remains dormant until certain conditions trigger reactivation. The absence of viral proteins during latency means that HSV-1 relies on host signaling pathways to initiate reactivation. One such pathway involves interleukin-1β (IL-1β), a key inflammatory cytokine. Previous studies have shown that IL-1β can induce HSV-1 reactivation by increasing neuronal excitability.
“Our findings identify the first viral protein required for herpes simplex virus to wake up from dormancy, and, surprisingly, this protein does so by triggering responses that should act against the virus,” Cliffe explained. “This is important because it gives us new ways to potentially prevent the virus from waking up and activating immune responses in the nervous system that could have negative consequences in the long term.”
With these new insights, scientists hope to develop treatments that prevent HSV-1 reactivation at its earliest stage. Inhibiting UL12.5 or blocking mitochondrial DNA release could be a strategy for reducing outbreaks and preventing the long-term inflammatory effects associated with recurrent infections.
The research has been published in the Proceedings of the National Academy of Sciences (PNAS), marking a significant step forward in understanding how herpes viruses manipulate the immune system.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Rebecca Shavit
Science & Technology Journalist | Innovation Storyteller
Based in Los Angeles, Rebecca Shavit is a dedicated science and technology journalist who writes for The Brighter Side of News, an online publication committed to highlighting positive and transformative stories from around the world. With a passion for uncovering groundbreaking discoveries and innovations, she brings to light the scientific advancements shaping a better future. Her reporting spans a wide range of topics, from cutting-edge medical breakthroughs and artificial intelligence to green technology and space exploration. With a keen ability to translate complex concepts into engaging and accessible stories, she makes science and innovation relatable to a broad audience.