Blood platelet test could save millions of Americans from heart attacks and strokes
A new genetic test called PRESS helps identify patients at high risk for cardiovascular events by measuring platelet hyperreactivity. Could this be the future of personalized heart disease prevention?

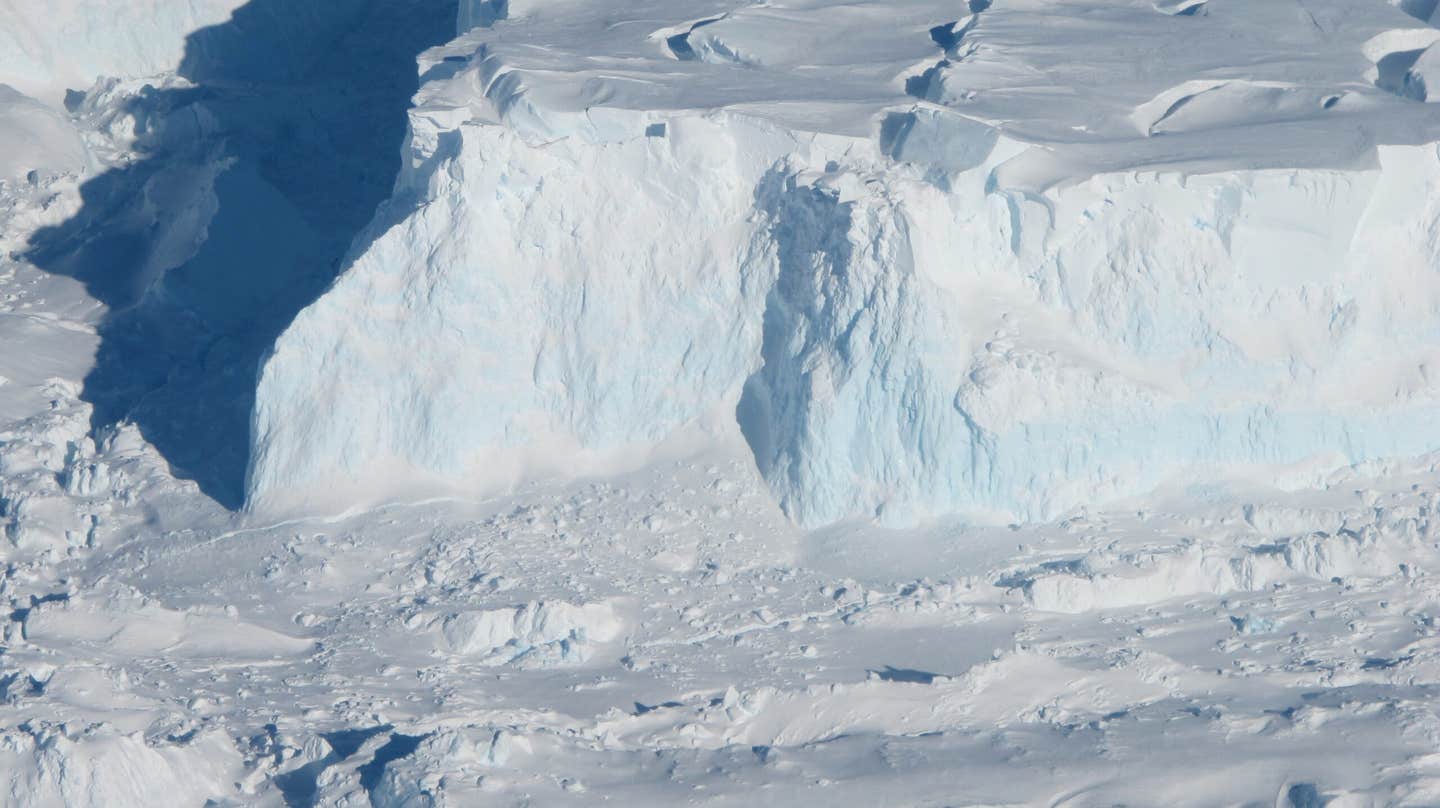
Currently, there isn’t a reliable, routine test to determine if your platelets are clumping too much, which complicates efforts to manage cardiovascular risk. (CREDIT: CC BY-SA 3.0)
Platelets, the small cell fragments circulating in your blood, are essential for healing injuries by clumping together to form blood clots. However, when platelets become hyperreactive, they can cause dangerous clots that block arteries, leading to heart attacks, strokes, and other cardiovascular issues, including peripheral artery disease. Millions of Americans are at risk from this abnormal clotting.
Currently, there isn’t a reliable, routine test to determine if your platelets are clumping too much, which complicates efforts to manage cardiovascular risk. The method most commonly used, known as platelet aggregometry, tends to produce results that vary significantly from one lab to another, making it impractical for widespread use.
A team of researchers at NYU Grossman School of Medicine is addressing this issue with a new approach. In a study published in Nature Communications, the researchers identified 451 genes with significant differences in activity between patients with hyperreactive platelets and those without. Using this information, they developed the Platelet Reactivity ExpresSion Score (PRESS), a genetic-based system that assesses platelet hyperreactivity and predicts cardiovascular risk.
Dr. Jeffrey Berger, the study’s lead author and director of the Center for the Prevention of Cardiovascular Disease at NYU Grossman School of Medicine, explains the significance of the findings: “Our results demonstrate that our new platelet-centric scoring system can, for the first time and across populations, circumvent aggregometry to reliably predict platelet hyperreactivity and the related risk of cardiovascular events.”
One of the major advantages of the PRESS system is its ability to identify hyperreactivity in both patients who are already at risk for heart attacks and in those who might not be aware of their future risk.
This advancement has the potential to reshape how physicians prescribe anti-platelet treatments like aspirin, which are often given based on general risk factors, such as high cholesterol or blood pressure—factors not directly related to platelet behavior. Dr. Berger notes, “PRESS promises to help physicians confine anti-platelet treatment to the people most likely to benefit: those with platelet hyperreactivity.”
Related Stories
Aspirin, widely used to reduce abnormal clotting, also increases the risk of bleeding, a significant drawback for many patients. A reliable method to identify who will benefit most from aspirin, without suffering adverse effects, has been needed in the field for some time. PRESS could be that solution.
The PRESS system’s development started with a shift away from traditional aggregometry techniques, which expose platelets to large doses of proteins that encourage clotting. These tests label platelets as dysfunctional if they don’t aggregate under these extreme conditions, but they weren’t designed to assess hyperreactivity. Dr. Berger’s team, and others in the field, opted for a different approach, one that exposes platelets to a much lower dose of epinephrine, a protein that encourages weaker aggregation.
In the study, the team defined hyperreactivity as when platelets exhibited 60% or more aggregation at a low epinephrine dose (0.4 μM). Using this method, they demonstrated that patients with hyperreactive platelets face a much higher risk of cardiovascular events.
These findings were reinforced by data from the Platelet Activity and Cardiovascular Events in PAD (PACE-PAD) clinical study, which tracks patients who have undergone procedures to open blocked arteries in the legs, known as lower extremity revascularization (LER).
Among the 254 patients studied, 17.5% exhibited hyperreactive platelets. These patients were more than twice as likely to experience major adverse cardiovascular and limb events (MACLE)—a composite measure that includes heart attacks, strokes, and limb amputations—within 30 days of their procedure compared to patients without hyperreactivity.
Despite the usefulness of this newer aggregometry method, the researchers aimed to create a test that could be easily implemented in everyday clinical settings, not just in specialized labs. This led to the creation of PRESS, which uses a genetic signature to predict platelet hyperreactivity, eliminating the need for complex blood collection techniques and other variables that complicate traditional aggregometry.
The team designed PRESS by analyzing genetic material from 129 patients in the PACE-PAD study before their LER procedures. The score was validated by comparing it with actual platelet aggregation data.
Further studies tested the score’s accuracy in other groups of patients, including participants in the Heart Attack Research Program. Among women undergoing coronary angiography, those with a higher PRESS score were more likely to have experienced a heart attack compared to those with stable coronary artery disease.
In patients with lower extremity atherosclerosis, PRESS also proved its predictive power. After tracking patients for an average of 18 months, researchers found that those with PRESS scores above the median had a 90% higher likelihood of experiencing a major cardiovascular event compared to those with lower scores.
This breakthrough offers exciting possibilities for personalizing cardiovascular care. “In current practice, anti-platelet therapy is not routinely recommended for the prevention of a first heart attack or stroke, but a platelet-based test would help to identify patients at highest risk,” says study co-author Dr. Tessa Barrett, an assistant professor at NYU Langone. PRESS could help physicians determine which patients would benefit most from anti-platelet therapies to prevent future cardiovascular events.
The PRESS score may mark a shift toward more individualized cardiovascular treatment, moving beyond broad risk factors and focusing on the underlying platelet activity that directly contributes to heart attacks and strokes. With its potential for wide application and the ability to identify patients at highest risk, this new tool could change the way cardiovascular disease is prevented and treated.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.