AI and high-speed video revolutionize diabetes and blood pressure screening
A new AI-driven system using high-speed video offers a non-invasive, contact-free method for detecting high blood pressure and diabetes with remarkable accuracy.
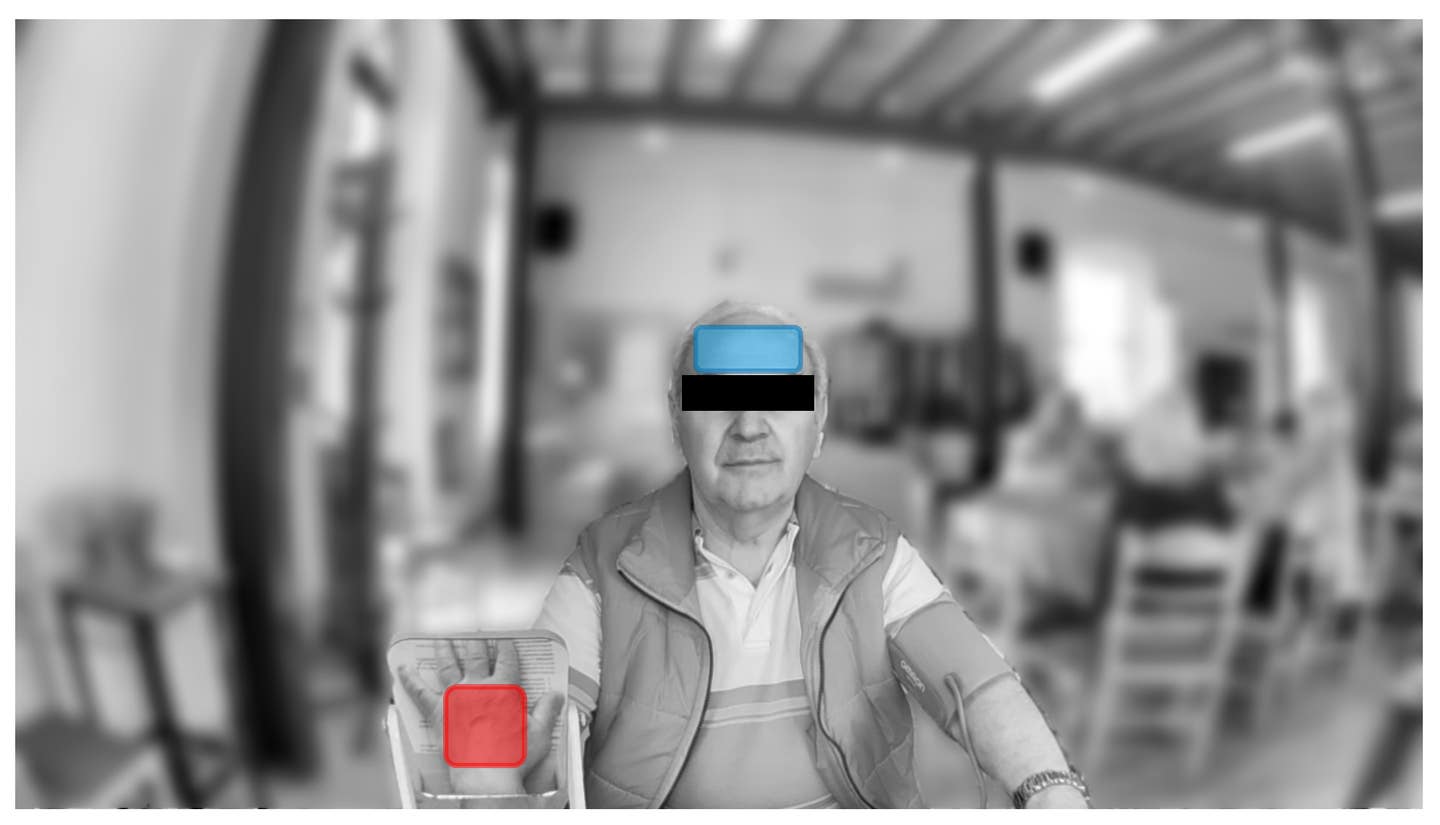
AI-powered high-speed video could transform diabetes and blood pressure screening. Sample image unrelated to this study. (CREDIT: MDPI)
A novel system combining high-speed video and AI algorithms could revolutionize health screenings for high blood pressure and diabetes. This innovation, presented at the American Heart Association’s Scientific Sessions 2024, provides a non-invasive, contact-free alternative to traditional blood tests and cuffs.
Ryoko Uchida, B.Sc. (Pharm.), from the University of Tokyo, emphasized its potential to bring medical monitoring into people’s homes. “This method may someday allow people to monitor their own health at home and could lead to early detection and treatment of high blood pressure and diabetes in people who avoid medical exams and blood tests,” Uchida explained.
Both conditions subtly alter blood flow in the face and hands. By recording these areas at 150 frames per second, researchers used an AI-powered algorithm to detect changes in pulse waves. The results were promising.
The system detected stage 1 hypertension with 94% accuracy, aligning with American Heart Association guidelines of 130/80 mm Hg or higher. It also identified above-normal blood pressure with 86% accuracy in 30 seconds and 81% in just 5 seconds. For diabetes, the system achieved 75% accuracy compared to hemoglobin A1c tests, which reflect average blood sugar over one to two months.
Uchida was surprised by the system's diabetes detection capability. “Some of the major complications of diabetes involve peripheral neuropathy and blood vessel damage. It makes sense that changes in blood flow would be a hallmark of diabetes,” she noted.
While these findings are exciting, there are hurdles to overcome. The system requires refinement to account for arrhythmias and other variables. Future versions could use simpler sensors for data collection, potentially integrated into everyday devices like smartphones or mirrors. The ultimate goal is to gain FDA approval for a home-use diabetes detection tool.
Related Stories
“Currently, the only way to confirm the diagnosis of diabetes is invasive blood tests. However, if it were to require only a non-invasive photo or video, that could be a game-changer,” Uchida said.
Eugene Yang, M.D., M.S., of the University of Washington, acknowledged the promise of non-invasive diagnostics but urged caution. “It is exciting to see more research that identifies ways to diagnose high blood pressure and diabetes non-invasively, two major risk factors for cardiovascular disease,” Yang said.
However, he noted the need for validation. “The referenced blood pressure monitor device used in this study, while cleared by the FDA, has not gone through appropriate validation protocols to ensure accuracy.”
Yang stressed that until thorough validation is complete, traditional methods remain the standard. “We must use validated devices for measuring blood pressure and glucose levels,” he added.
The study, which involved 215 adults (average age 64, 36% female), primarily included Japanese and other Asian participants. Sixty-two had high blood pressure, 88 had normal readings, and 44 had diabetes or elevated HbA1c levels. Data was gathered from 22 facial and 8 palm regions in controlled hospital settings.
Researchers acknowledge the study's limitations. It focused on a predominantly Japanese population and may not apply to other groups. Lighting conditions and participant movement could also affect results. Further studies in diverse populations and real-world settings are needed.
Despite these challenges, the potential impact of this technology is undeniable. It offers a glimpse into a future where managing chronic conditions could be as simple as taking a selfie.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Joshua Shavit
Science & Technology Writer | AI and Robotics Reporter
Joshua Shavit is a Los Angeles-based science and technology writer with a passion for exploring the breakthroughs shaping the future. As a contributor to The Brighter Side of News, he focuses on positive and transformative advancements in AI, technology, physics, engineering, robotics and space science. Joshua is currently working towards a Bachelor of Science in Business Administration at the University of California, Berkeley. He combines his academic background with a talent for storytelling, making complex scientific discoveries engaging and accessible. His work highlights the innovators behind the ideas, bringing readers closer to the people driving progress.