A patient’s blood could regenerate their broken bones, study finds
Scientists develop blood-based regenerative materials, enabling personalized implants to heal bones and tissues.
Researchers have created a groundbreaking material from blood, offering new hope for personalized regenerative therapies. (CREDIT: iStock Photo)
As the global population ages, the demand for regenerative therapies grows, yet replicating the natural complexity of the body’s healing processes remains a daunting challenge. While techniques like stem cell therapies, organoids, and gene editing show promise, issues such as safety, reproducibility, and efficiency limit their widespread use.
For injuries to tissues like bone, skin, and ligaments, current gold-standard treatments rely on grafts, which come with significant drawbacks—pain, donor site morbidity, and limited availability. A novel approach rooted in the body’s natural processes may provide a way forward.
Blood’s Role in Regeneration
The human body has evolved to repair small injuries with remarkable efficiency, primarily through a process that begins with the formation of the regenerative hematoma (RH). This solid clot forms from liquid blood and serves as a dynamic environment filled with cells, macromolecules, and growth factors critical for healing.
Platelets in the RH release pro-inflammatory cytokines and growth factors such as vascular endothelial growth factor (VEGF) and transforming growth factor-β (TGF-β).
Meanwhile, leukocytes fight infections, and monocytes transform into macrophages that secrete additional factors like interleukins and tumor necrosis factor-α (TNF-α). These processes stimulate cell recruitment, vascularization, and granulation, enabling the repair of tissues like bone.
Scientists have long sought to harness the regenerative potential of blood. Materials such as fibrin scaffolds and platelet-rich plasma (PRP) have been developed to aid healing.
While PRP can be prepared from a patient’s blood, it requires large volumes, exhibits variable properties, and often depends on external agents like bovine thrombin to form gels. These limitations, along with the exclusion of critical components like erythrocytes and albumin, have led researchers to explore the use of whole blood as a living, bioactive material.
Innovations in Blood-Based Materials
Pioneering studies have demonstrated the potential of blood-derived materials. For instance, integrating blood clots with calcium phosphate composites significantly improved bone formation in animal models. Similarly, chitosan-blood composites and blood-polymer gels have shown promise for wound repair and hemostasis.
Related Stories
Despite these advances, practical challenges—such as controlling clot properties and material processing—have restricted their broader application. Scientists now aim to directly interact with the endogenous molecules and processes in the RH to enhance and accelerate natural regeneration.
A breakthrough approach involves self-assembling peptides—molecules that form nanoscale structures and display bioactive signals. Researchers have developed peptide amphiphiles (PAs) capable of co-assembling with proteins to create composite nanostructures.
By modifying PA structures, scientists can tailor the mechanical properties and incorporate additional components like biopolymers or graphene oxide. These innovations allow the design of materials that mimic the RH’s complexity and functionality.
A New ‘Biocooperative’ Material
Researchers from the University of Nottingham have taken a major step forward by creating a material derived from a patient’s own blood. Using peptide molecules, the team engineered a self-assembling system that combines peptides with whole blood to form a regenerative material. This “biocooperative” approach leverages the body’s natural healing mechanisms rather than attempting to replicate them artificially.
“For years, scientists have struggled to recreate the complexity of the natural regenerative environment,” said Professor Alvaro Mata, a leading researcher in biomedical engineering. “Our approach uses the body’s own regenerative mechanisms as fabrication steps to engineer materials that enhance healing.”
The resulting material retains key functions of the RH, such as platelet behavior, growth factor generation, and cell recruitment.
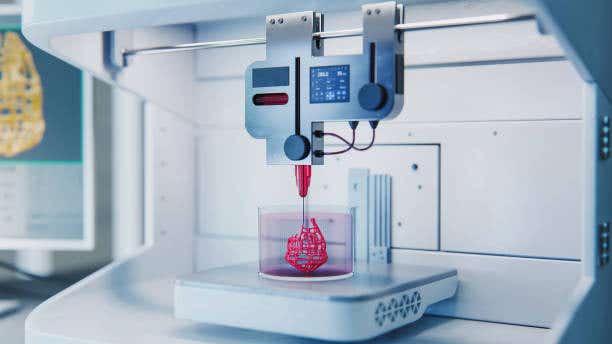
Additionally, it can be easily assembled, manipulated, and even 3D-printed to create personalized implants. In animal models, the material demonstrated the ability to repair bone using the animal’s own blood, paving the way for patient-specific regenerative therapies.
Dr. Cosimo Ligorio, a co-author of the study, highlighted the clinical potential: “Blood is practically free and easily obtainable in large volumes. Our aim is to establish a toolkit that clinicians can use to transform patients’ blood into accessible and tunable regenerative implants.”
Transforming Regenerative Medicine
This innovation represents a significant leap in regenerative medicine. By using the natural properties of blood and self-assembling peptides, scientists have developed a material that not only mimics the RH but enhances its structural and functional properties. Unlike previous approaches that relied on synthetic materials or external agents, this method integrates seamlessly with the body’s biology.
The material’s versatility also opens new possibilities for personalized medicine. For example, it can be customized to address specific injuries or diseases and adapted for use in different tissue types. The ability to 3D-print these materials further enhances their practicality, offering a scalable solution for complex medical challenges.
However, much work remains before these materials reach clinical settings. The researchers stress the need for further studies to optimize the material’s properties, ensure its safety, and evaluate its long-term efficacy. Nonetheless, the potential for transforming regenerative medicine is clear.
The future of regenerative therapies lies in harnessing the body’s innate healing capabilities. By combining cutting-edge biomaterials with natural processes, scientists are creating a new class of therapies that could revolutionize the treatment of injuries and diseases. The ability to turn a patient’s own blood into a regenerative implant offers a glimpse of what personalized medicine could achieve.
As Professor Mata explained, “This approach not only enhances healing but also aligns with the principles of biology, opening new avenues for safe and effective therapies.”
With ongoing research and development, these innovations could soon bridge the gap between regenerative medicine’s potential and its practical application, offering hope for millions worldwide.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Rebecca Shavit
Science & Technology Journalist | Innovation Storyteller
Based in Los Angeles, Rebecca Shavit is a dedicated science and technology journalist who writes for The Brighter Side of News, an online publication committed to highlighting positive and transformative stories from around the world. With a passion for uncovering groundbreaking discoveries and innovations, she brings to light the scientific advancements shaping a better future. Her reporting spans a wide range of topics, from cutting-edge medical breakthroughs and artificial intelligence to green technology and space exploration. With a keen ability to translate complex concepts into engaging and accessible stories, she makes science and innovation relatable to a broad audience.



