New ‘drug-factory’ implants successfully kill many types of cancer, study finds
Tiny implants delivering cytokines directly to tumors offer safer, effective cancer therapy, soon entering human clinical trials.

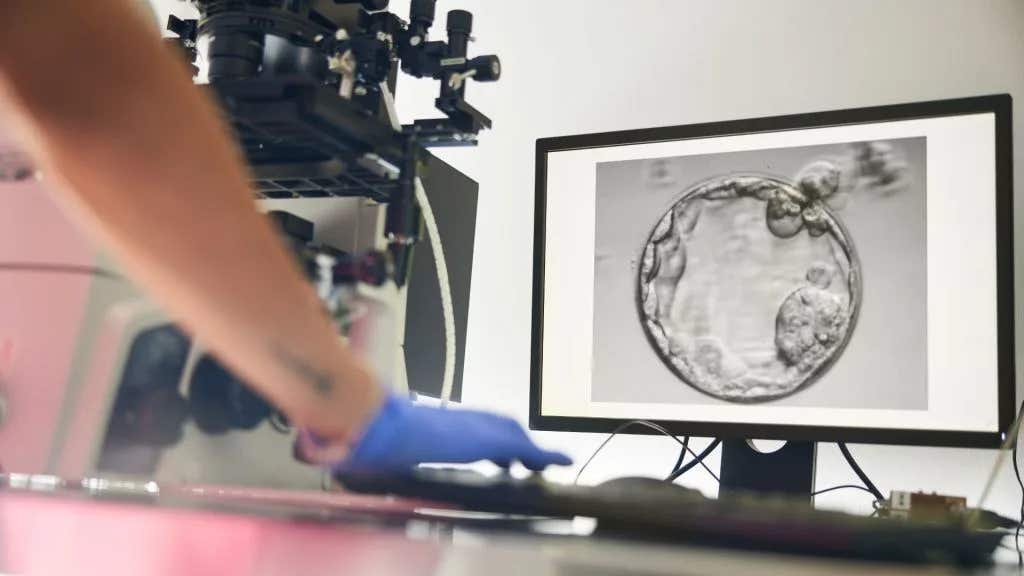
Researchers developed microscopic implants producing natural cytokines directly at tumor sites, dramatically improving cancer treatment outcomes. (CREDIT: Jeff Fitlow/Rice University)
Cancer treatment has long faced a challenging trade-off: therapies strong enough to eliminate tumors often cause severe side effects. One promising solution involves cytokines, natural proteins that stimulate your immune system to attack cancer cells.
However, conventional cytokine therapies have significant limitations. Scientists from Rice University and Baylor College of Medicine are overcoming these hurdles by developing tiny implants that produce cytokines directly at tumor sites.
Understanding Cytokines and Their Challenges
Cytokines act as messengers in your immune system, triggering responses that fight infections or cancers. Specifically, interleukin-2 (IL-2) boosts the activity of immune cells called T cells, critical for destroying cancer cells.
Since 1992, IL-2 has received FDA approval under names like Aldesleukin for melanoma and kidney cancer treatment. Yet, traditional methods involve high doses of IL-2 injected intravenously, causing dangerous side effects such as vascular leak syndrome. This condition results in fluid buildup damaging vital organs like your heart and kidneys.
Moreover, IL-2 rapidly disappears from your bloodstream, meaning high doses are necessary to fight tumors effectively. Repeated high doses often trigger your immune system to produce antibodies against the treatment itself, further reducing its effectiveness.
A New Approach: Cytokine Factories
To overcome these drawbacks, researchers developed "cytokine factories"—microscopic beads loaded with thousands of engineered cells that naturally produce IL-2. Each bead, just 1.5 millimeters wide, continuously delivers IL-2 directly to tumor sites, significantly reducing systemic side effects.
Related Stories
In studies published in journals like Clinical Cancer Research, researchers implanted these cytokine-producing beads next to tumors in mice with ovarian, colorectal, and mesothelioma cancers. Remarkably, ovarian and colorectal tumors vanished within days. In mice with aggressive mesothelioma—a cancer of the lung lining often caused by asbestos exposure—over half the tumors disappeared using only the implants.
Even more impressively, when cytokine factories were combined with checkpoint inhibitor drugs targeting proteins like PD-1, every mesothelioma tumor treated disappeared completely.
Dr. Bryan Burt, chief of Baylor’s Division of Thoracic Surgery, highlighted the significance, stating, "It's very hard to treat mesothelioma tumors in mice, just as it is in humans. Our data show regional delivery produces very effective treatment responses. I've never seen such efficacy in eradicating mesothelioma tumors in mice."
Why Localized Delivery Matters
Local administration directly into tumor regions like the pleural cavity—the space around your lungs—offers major advantages. IL-2 concentrations in these localized treatments remain about 100 times higher than in your bloodstream. This method maintains therapeutic effects without causing widespread toxicity.
In a clinical trial with ovarian cancer patients receiving IL-2 directly into the peritoneal cavity, side effects were significantly reduced compared to traditional treatments.
Amanda Nash, a Rice University graduate student involved in developing the cytokine factories, emphasized the platform's potential: "From the beginning, our objective was to develop a platform therapy useful for multiple immune disorders or cancers."
Clinical Trials and Future Directions
Encouraged by these results, researchers are rapidly moving toward human trials. A spinout company, Avenge Bio, has secured FDA approval to start trials for ovarian cancer patients later this year. Additionally, researchers are preparing trials targeting mesothelioma and other lung cancers spreading within the chest cavity.
Dr. Omid Veiseh, a Rice bioengineer leading this research, described the upcoming clinical plans: "In the next couple of months, they expect to begin treating patients with these IL-2 cytokine factories." Meetings with the FDA have already laid groundwork for these promising trials.
Beyond cancer, Veiseh and colleagues received an American Heart Association grant to explore cytokine implants for heart attack recovery. This expansion into heart disease highlights the broad therapeutic possibilities of the technology.
Safety and Efficacy Confirmed
Preclinical studies confirmed these cytokine factories are both safe and effective. Tests involving nonhuman primates showed the implants triggered strong immune responses without toxic effects. Pharmacokinetic modeling—used to predict how the therapy works in humans—also indicated the treatment should translate successfully to clinical use.
Such precise control over dosage and duration addresses longstanding challenges of cytokine therapy, promising fewer complications and better patient outcomes.
A Versatile Therapy Platform
These cytokine factories represent a major breakthrough in cancer immunotherapy. By delivering cytokines directly to tumors at controlled rates, they harness your body's immune system effectively while minimizing harmful side effects. This approach could revolutionize treatments for multiple cancer types, improving quality of life and survival rates for patients.
As clinical trials begin, researchers remain hopeful this innovative treatment could soon become a reality for many patients. The platform's versatility may also lead to new therapies for various immune-related conditions, further demonstrating its enormous potential.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.