Breakthrough new procedure eliminates the need for insulin in less than an hour
Type 2 diabetes affects more than 37 million Americans, with over 90% of these individuals battling this life-long chronic condition.

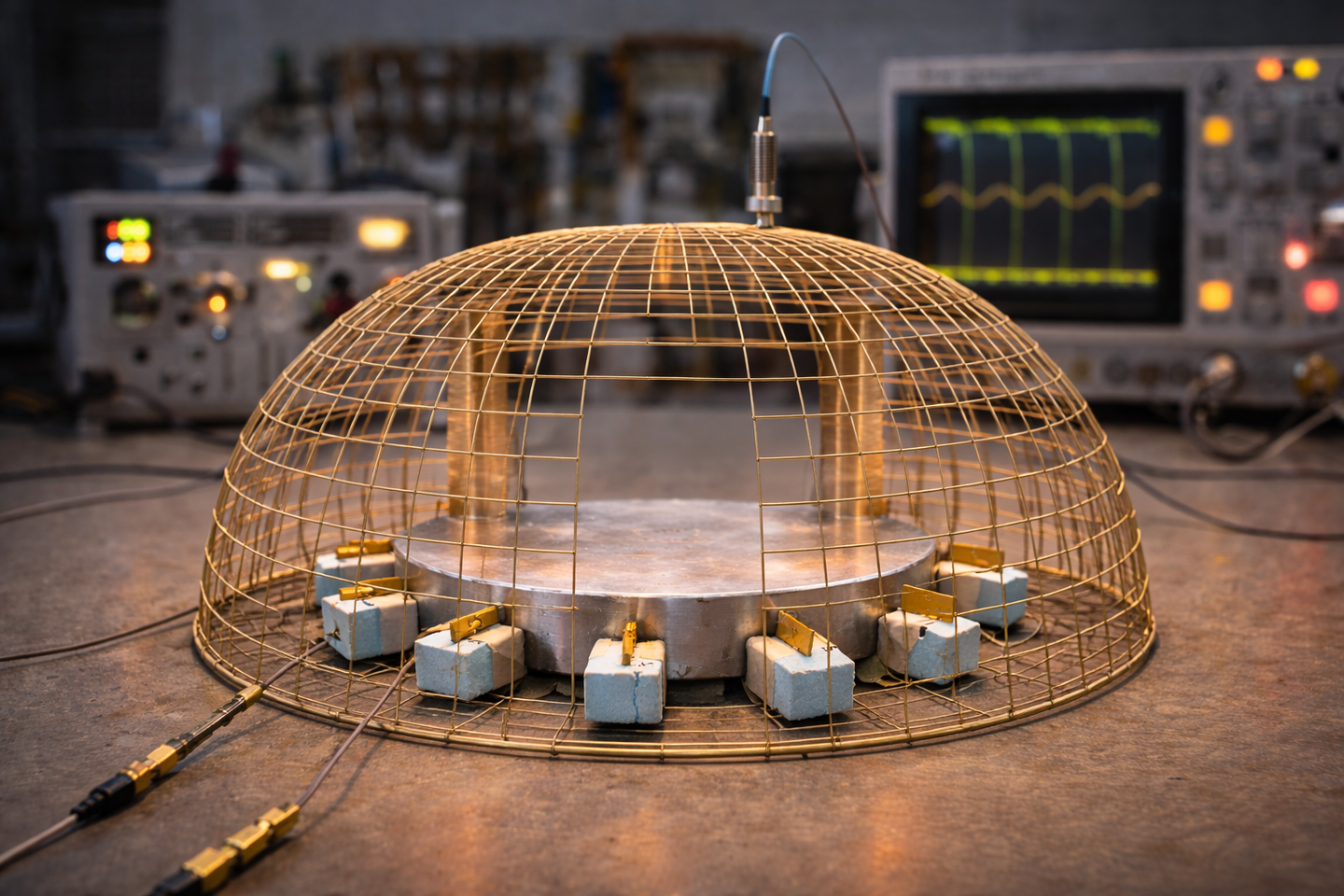
Electrical stimulation of the duodenum, the first segment of the small intestine, may soon offer a revolutionary outpatient procedure for Type 2 diabetes patients. (CREDIT: CC BY-SA 3.0)
Electrical stimulation of the duodenum, the first segment of the small intestine, may soon offer a revolutionary outpatient procedure for Type 2 diabetes patients. This promising approach could enable patients to achieve glycemic control and potentially discontinue insulin use, according to a preliminary study conducted at Amsterdam University Medical Center.
Led by Celine Busch, a PhD student in gastroenterology, and Dr. Jacques Bergman, a professor specializing in gastrointestinal endoscopy, the research is paving the way for a new treatment paradigm.
Type 2 diabetes affects more than 37 million Americans, with over 90% of these individuals battling this chronic condition. Traditional treatment methods usually involve glucose-lowering medications or insulin injections, both of which come with side effects such as low blood sugar and weight gain. The study's findings suggest a potential breakthrough: a single, outpatient procedure that offers lasting glycemic control without the need for daily medication.
“The potential for controlling diabetes with a single endoscopic treatment is spectacular,” Busch remarked, highlighting the significance of this research.
Earlier investigations have examined the effects of ablation, a technique that uses heat to alter the lining of the small intestine. This line of inquiry was inspired by observations that patients undergoing gastric bypass surgery often experienced improved insulin control immediately after the procedure, even before losing any weight. Such outcomes indicated that bypassing this part of the small intestine could play a crucial role in managing Type 2 diabetes.
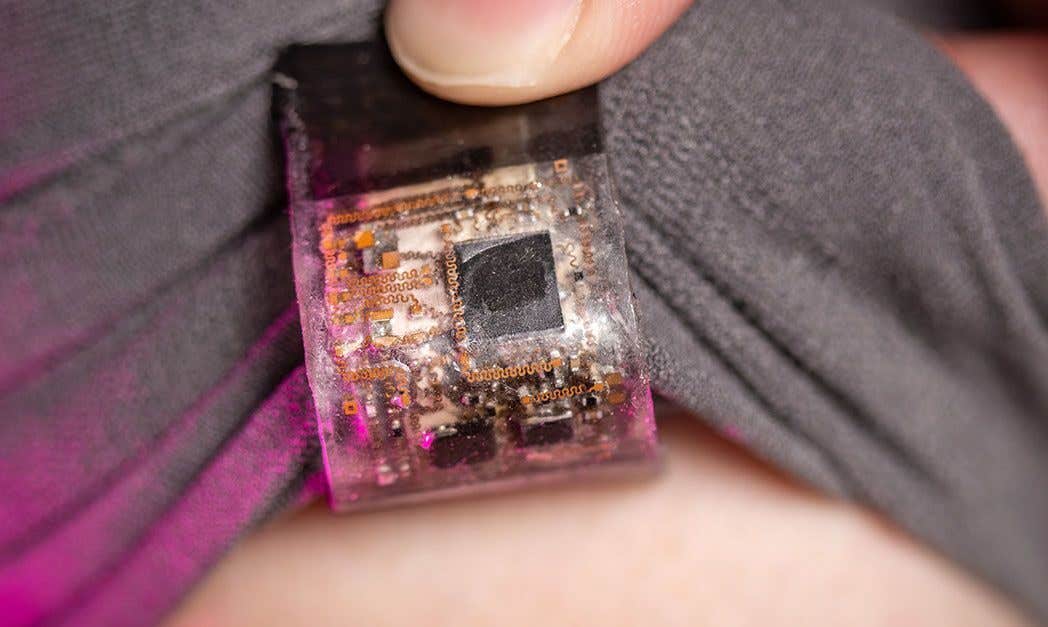
In the current study, 14 participants underwent an endoscopic procedure lasting about an hour. During this process, alternating electrical pulses were delivered to the lining of the small intestine just below the stomach. Following the procedure, patients were sent home the same day and placed on a calorie-controlled liquid diet for two weeks. Afterward, they began taking semaglutide, a diabetes medication, gradually increasing the dosage to 1 mg per week.
While semaglutide alone can sometimes help patients with Type 2 diabetes discontinue insulin, this happens in only about 20% of cases. However, in this study, 12 out of 14 patients—approximately 86%—maintained good glycemic control without insulin for a year.
Related Stories
This remarkable outcome suggests that the procedure itself, not just the medication, played a significant role in achieving these results. To further validate these findings, the researchers are now preparing to conduct a double-blind randomized controlled trial.
“This one procedure is ‘disease-modifying’ in that it reverses the body’s resistance to its own insulin, the root cause of Type 2 diabetes,” Dr. Bergman explained. The research team theorizes that chronic exposure to a high-sugar, high-calorie diet induces changes in the lining of the small intestine, leading to insulin resistance. By rejuvenating the tissue in this part of the intestine, the procedure may enhance the body's ability to respond to its own insulin, particularly in patients who still produce some insulin.
Despite these promising results, the study remains in its early stages. The researchers are eager to proceed with a double-blind randomized controlled trial to further explore the procedure's potential.
The procedure in question, known as duodenal mucosal resurfacing (DMR), involves delivering electrical pulses to the duodenum's lining. A specialized catheter administers this electrical energy, creating a controlled injury to the mucosal layer. This injury prompts tissue regeneration, thereby enhancing the body's insulin response.
The procedure is performed under sedation and typically takes about an hour, after which patients can return home the same day. They are then placed on a calorie-controlled liquid diet for two weeks, followed by the gradual introduction of semaglutide.
"DMR is a promising new therapy that could potentially help millions of people with Type 2 diabetes who struggle to manage their blood sugar levels with traditional medications," Busch emphasized. She reiterated the procedure’s significance, describing it as “disease-modifying” because of its ability to reverse the underlying cause of Type 2 diabetes.
Endogenex, a Minnesota-based company that owns the technology used for the DMR procedure, fully funded the study. Dr. Bergman serves on Endogenex's advisory board, and the company has already begun working on a double-blind randomized controlled trial to test the results further.
While the study's results are encouraging, some experts have voiced concerns about the long-term safety and efficacy of the DMR procedure. Dr. Kenneth Snow, an endocrinologist and clinical professor of medicine at the University of Washington, expressed cautious optimism. He noted, “Type 2 diabetes is a complex disease that requires a multifaceted approach to treatment. While the DMR procedure may provide short-term benefits, it remains to be seen whether it will be a safe and effective long-term solution for patients.”
Other experts have also pointed out that the DMR procedure is not without risks, including the potential for bleeding, infection, and damage to surrounding organs. Additionally, the procedure is currently available at only a limited number of medical centers globally, which may limit accessibility for some patients.
Despite these concerns, the researchers remain hopeful about the potential of DMR to revolutionize Type 2 diabetes treatment. “This is just the beginning of what could be a major breakthrough in the field of diabetes research,” Busch stated. She and her colleagues are excited to continue studying the long-term effects of the DMR procedure and explore new avenues to improve the lives of those living with Type 2 diabetes.
As the medical community awaits further results from ongoing trials, the prospect of a one-time procedure that could alleviate the burden of daily insulin injections offers a glimpse of a future where Type 2 diabetes might be managed more effectively and with fewer side effects.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.