Revolutionizing Cancer Treatment: Turning Cancer Cells into Self-Destructing Trojan Horses
Personalized cancer medicines often fail due to cancer’s inherent diversity and heterogeneity. Even effective frontline therapies eventually face resistance.
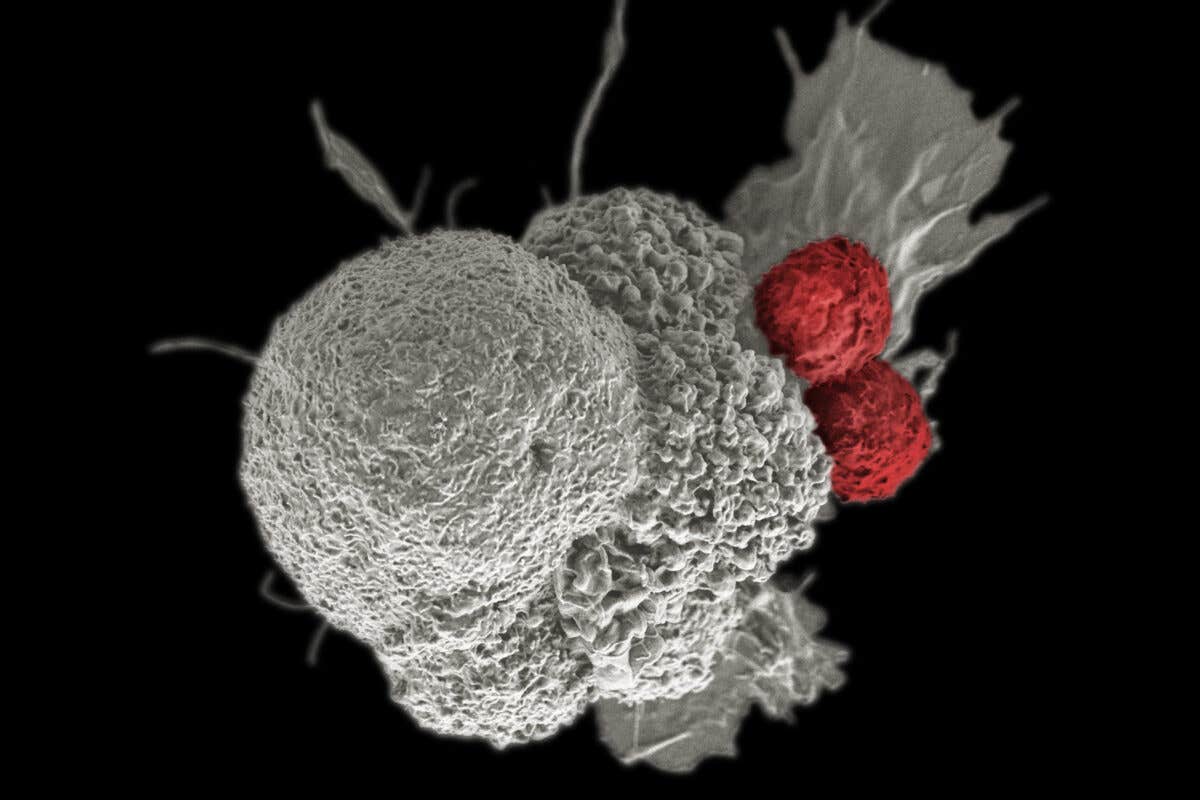
Researchers at Penn State have discovered a way to reprogram cancer evolution, creating tumors that are easier to treat.(CREDIT: Creative Commons)
Cancer treatment often feels like a game of Whac-A-Mole. The disease develops resistance to therapies, leaving clinicians perpetually one step behind. However, researchers at Penn State have discovered a way to reprogram cancer evolution, creating tumors that are easier to treat. Their breakthrough involves a modular genetic circuit that turns cancer cells into a "Trojan horse," causing them to self-destruct and eliminate nearby drug-resistant cells.
The team's findings, published in Nature Biotechnology, offer a promising new approach to cancer treatment. The researchers have also filed a provisional patent application for their innovative technology.
“This idea was born out of frustration. We’re not doing a bad job of developing new therapeutics to treat cancer but how can we think about potential cures for more late-stage cancers?” said Justin Pritchard, Dorothy Foehr Huck and J. Lloyd Huck Early Career Entrepreneurial Associate Professor of Biomedical Engineering and senior author on the paper. “Selection gene drives are a powerful new paradigm for evolution-guided anticancer therapy. I love the idea that we can use a tumor’s inevitability of evolution against it.”
Personalized cancer medicines often fail due to cancer's inherent diversity and heterogeneity, Pritchard explained. Even effective frontline therapies eventually face resistance, allowing cancer to return. This forces clinicians to restart the treatment process with new drugs, only for resistance to emerge again. This cycle continues until no further options are available.
“You’re playing a game of Whac-A-Mole. You don’t know which mole is going to pop up next, so you don’t know what is going to be the best drug to treat the tumor. We’re always on our back foot, unprepared,” said Scott Leighow, a postdoctoral scholar in biomedical engineering and lead author of the study.
The researchers speculated if they could get ahead of the cancer cells. Could they eliminate resistance mechanisms before the cells evolve? Could they force a specific "mole" to appear, one they are prepared to combat?
What began as a thought experiment is now a promising reality. The team designed a modular circuit, or dual-switch selection gene drive, and introduced it into non-small lung cancer cells with an EGFR gene mutation—a known target for existing drugs.
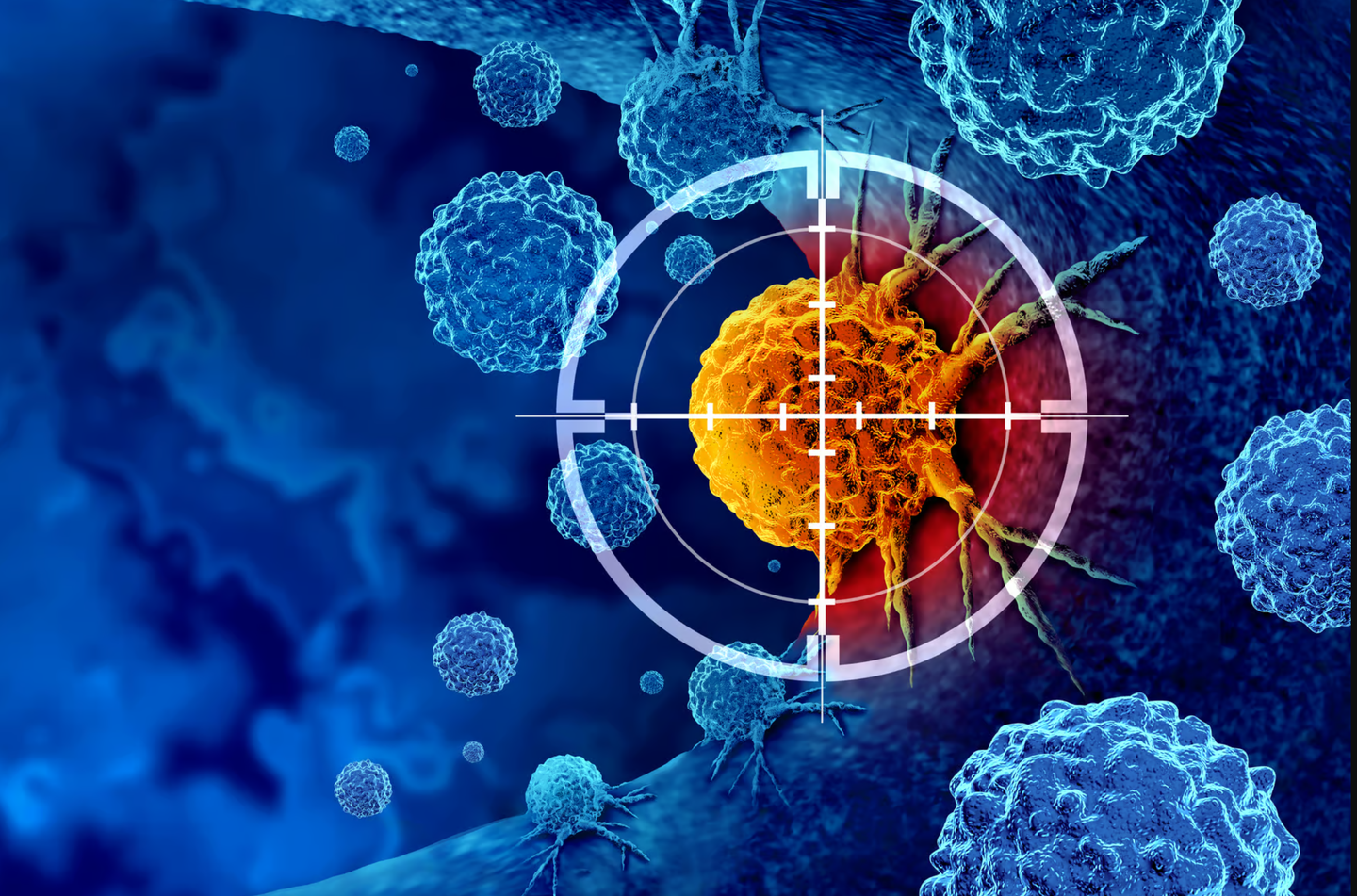
The circuit includes two genes, or switches. The first switch acts as a selection gene, allowing researchers to toggle drug resistance on and off. With the first switch turned on, the genetically modified cells become temporarily resistant to a specific drug. When treated with this drug, the native drug-sensitive cancer cells die off, leaving behind the modified, drug-resistant cells and a small population of native resistant cells. The modified cells eventually outgrow the native resistant cells, preventing further resistance evolution.
The resulting tumor predominantly consists of genetically modified cells. When the first switch is turned off, these cells become drug-sensitive again. The second switch, the therapeutic payload, contains a suicide gene. This gene enables the modified cells to produce a diffusible toxin that kills both the modified and neighboring unmodified cells.
“It not only kills the engineered cells, but it also kills the surrounding cells, namely the native resistant population,” Pritchard said. “That’s critical. That’s the population you want to get rid of so that the tumor doesn’t grow back.”
The researchers first simulated tumor cell populations and used mathematical models to test their concept. They then cloned each switch separately into viral vectors and tested them in human cancer cell lines. After confirming functionality, they combined the two switches into a single circuit and tested it again. When the circuit worked in vitro, they conducted experiments in mice.
However, the team wanted to ensure the circuit's robustness against various genetic resistance variants. They stress-tested the system using complex genetic libraries of resistance variants to see if the gene drive could counter all possible resistance mechanisms in cancer cell populations.
The results were promising: Even a few engineered cells could dominate the cancer cell population and eradicate high levels of genetic heterogeneity. Pritchard highlighted this as a major strength of the paper, both conceptually and experimentally.
“The beauty is that we’re able to target the cancer cells without knowing what they are, without waiting for them to grow out or resistance to develop because at that point it’s too late,” Leighow said.
The researchers are now working on translating this genetic circuit for safe and selective delivery into growing tumors and eventually metastatic disease.
Other contributors to the paper include Marco Archetti, associate professor of biology; Shun Yao, a postdoctoral scholar in biology; Ivan Sokirniy, graduate student at the Huck Institutes of the Life Sciences; and Joshua Reynolds and Zeyu Yang, members of the Department of Biomedical Engineering. Co-author Haider Inam, a doctoral student in biomedical engineering during the research, is now a research scientist at the Broad Institute of MIT and Harvard. Dominik Wodarz, professor at the University of California, San Diego, also contributed to the paper.
The Huck Institutes of Life Sciences’ HITS Fund, the National Cancer Institute, and the National Institute of Biomedical Imaging and Bioengineering Trailblazer award supported this work.
This groundbreaking approach marks a significant step forward in cancer treatment. By reprogramming cancer evolution, researchers have paved the way for more effective and targeted therapies, offering new hope for patients facing drug-resistant cancers.
Note: Materials provided above by the The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get the Brighter Side of News' newsletter.
Joshua Shavit
Science & Technology Writer | AI and Robotics Reporter
Joshua Shavit is a Los Angeles-based science and technology writer with a passion for exploring the breakthroughs shaping the future. As a contributor to The Brighter Side of News, he focuses on positive and transformative advancements in AI, technology, physics, engineering, robotics and space science. Joshua is currently working towards a Bachelor of Science in Business Administration at the University of California, Berkeley. He combines his academic background with a talent for storytelling, making complex scientific discoveries engaging and accessible. His work highlights the innovators behind the ideas, bringing readers closer to the people driving progress.