New antibody innovation looks to revolutionize cancer treatment
Discover how precision immunotherapy is revolutionizing cancer treatment with innovative antibody technologies for safer, tailored therapies.

Groundbreaking advances in precision immunotherapy, feature a 3-in-1 antibody design that enhances cancer treatment safety, speed, and effectiveness. (CREDIT: CC BY-SA 4.0)
Cancer treatment has entered a revolutionary phase with advancements in immunotherapy, a field that employs the immune system to target and destroy tumors.
Among these innovations, checkpoint inhibitors have made significant strides by enabling T cells to attack cancer cells effectively, enhancing patient survival rates. However, limitations like antigen escape—a phenomenon where cancer cells evade immune detection—pose challenges to current therapies such as tumor-targeted antibodies and CAR-T cells.
Scientists are now exploring versatile alternatives like cancer vaccines and immune-activating therapies that can generate anti-tumor responses against a broader range of targets.
Recent developments highlight the potential of antibody-drug conjugates (ADCs) and other cutting-edge technologies to overcome these obstacles, paving the way for more efficient, patient-tailored cancer treatments.
Checkpoint inhibitors, which amplify existing immune responses against tumors, have shown the ability to cure some critically ill patients. Meanwhile, cancer vaccines and agonistic immunotherapies work by inducing immune responses against tumor-specific antigens presented by major histocompatibility complexes (MHC).
These methods complement existing therapies but face challenges such as poor bioavailability, skewed immune responses, and variability in peptide or protein production when using mRNA-based platforms.
Nanoparticle-based systems and lipid-based formulations, while promising, often struggle with suboptimal pharmacokinetics and delivery issues. This is where ADCs, which combine precision targeting with payload delivery, emerge as a promising solution.
By leveraging antibody-based targeting domains, ADCs can enhance antigen delivery and improve immune responses, addressing the limitations of conventional methods.
Related Stories
The Role of CD40 in Immune Activation
Targeting the CD40 receptor has garnered attention for its role in stimulating the immune system. CD40 agonistic antibodies mimic the natural interaction between the CD40 receptor and its ligand, CD40L, triggering immune responses through cytokine release and T-cell activation. This approach promotes a Th1-dominant immune response, critical in fighting cancer.
However, using high-affinity agonistic antibodies comes with risks, including liver dysfunction, cytokine release syndrome, and immune exhaustion. Combining CD40 targeting with chemotherapy or intra-tumoral administration has shown promise in enhancing efficacy.
Researchers are also exploring bispecific antibody formats to focus CD40 activation within the tumor microenvironment. These advancements aim to minimize side effects while maximizing therapeutic impact.
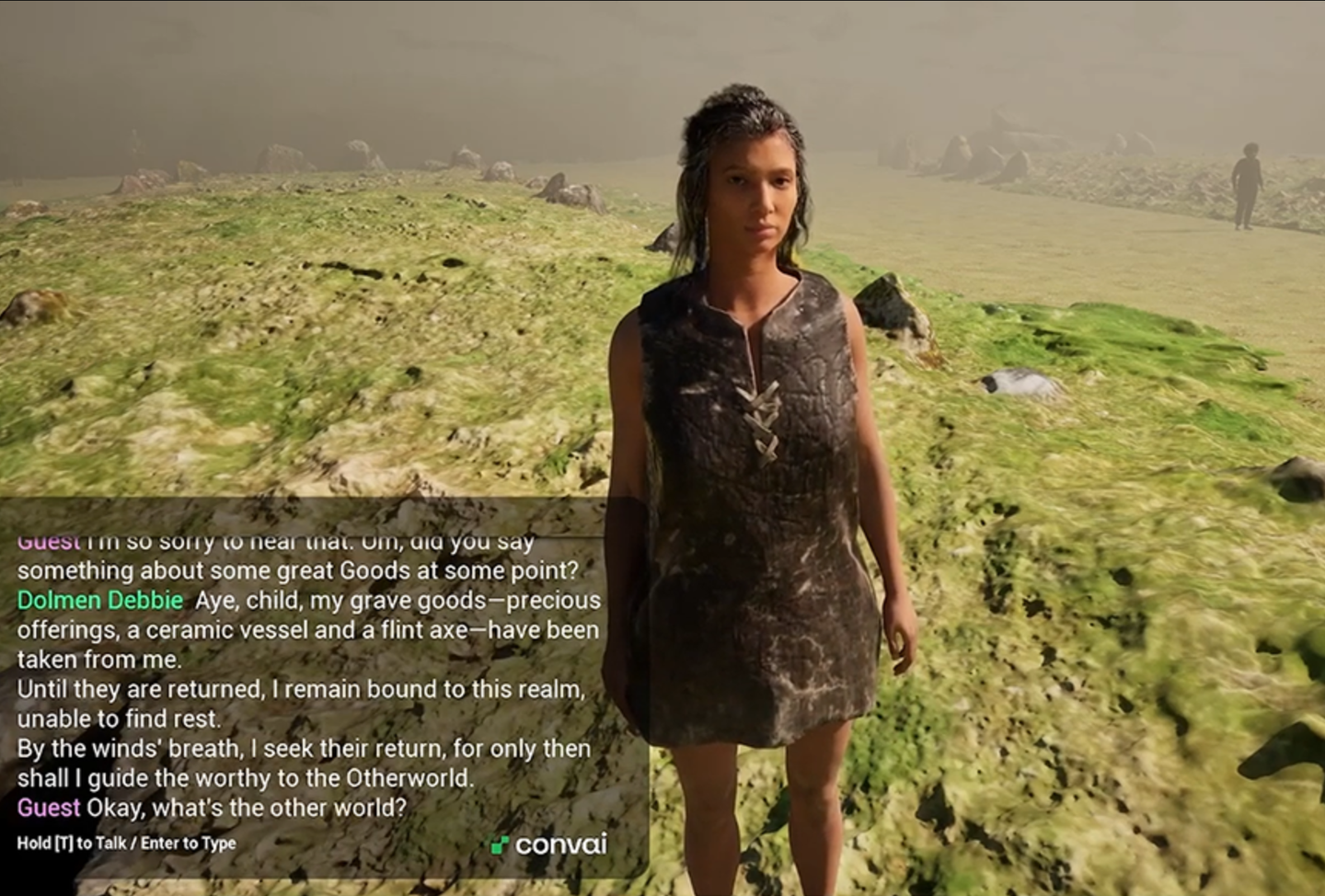
A groundbreaking approach involves Adaptive Drug Affinity Conjugate (ADAC) technology, which allows flexible and rapid drug cargo delivery to CD40-expressing cells.
Unlike traditional ADCs, ADAC uses a bispecific design that binds synthetic peptides with high affinity. This method enables in-hospital customization of patient-specific peptides, combining vaccination with immune activation in a single step.
Initial studies demonstrated extended drug half-life, improved targeting, and enhanced T-cell responses both in vitro and in vivo. While further work is needed to refine this technology for clinical use, it offers a promising pathway for personalized cancer immunotherapy.
Precision Medicine Takes Center Stage
Researchers from Uppsala University and KTH Royal Institute of Technology have introduced a novel antibody with a “3-in-1 design” that combines targeting, drug delivery, and immune activation. This precision medicine breakthrough focuses on neoantigens—mutations unique to cancer cells—to train the immune system to recognize and attack tumors.
The antibody simultaneously delivers tumor-specific materials to immune cells and activates those cells to strengthen the T-cell response. Preclinical studies in mice demonstrated prolonged survival and even complete cancer remission at higher doses, suggesting the approach is safer and more effective than traditional treatments.
Customizing cancer treatments often involves high costs and lengthy development times. However, the new antibody design addresses these challenges. Its modular structure includes a bispecific antibody produced in bulk and a synthetic peptide tailored to individual tumors. This approach reduces production costs and shortens the time from diagnosis to treatment.
"The advantage of our drug is that it is easy to produce on a larger scale, yet can be tailored to the patient’s specific tumor," said Johan Rockberg, a professor at KTH Royal Institute of Technology and co-author of the study. The researchers aim to make precision cancer treatment more accessible while maintaining its adaptability for individual patients.
The next phase involves optimizing the manufacturing process and conducting safety studies to prepare for clinical trials. By enabling personalized immunotherapy that is both efficient and cost-effective, this innovative approach holds promise for transforming cancer treatment.
The technology’s ability to combine speed, flexibility, and scalability positions it as a potential game-changer in oncology.
As these advancements progress, the future of cancer treatment seems increasingly within reach, offering hope to patients worldwide.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.