Major new study finds gut health is critical to the prevention and cure of Alzheimer’s disease
Alzheimer’s remains a major health concern, being the predominant diagnosis for dementia patients and ranking sixth as a cause of death in the U.S.

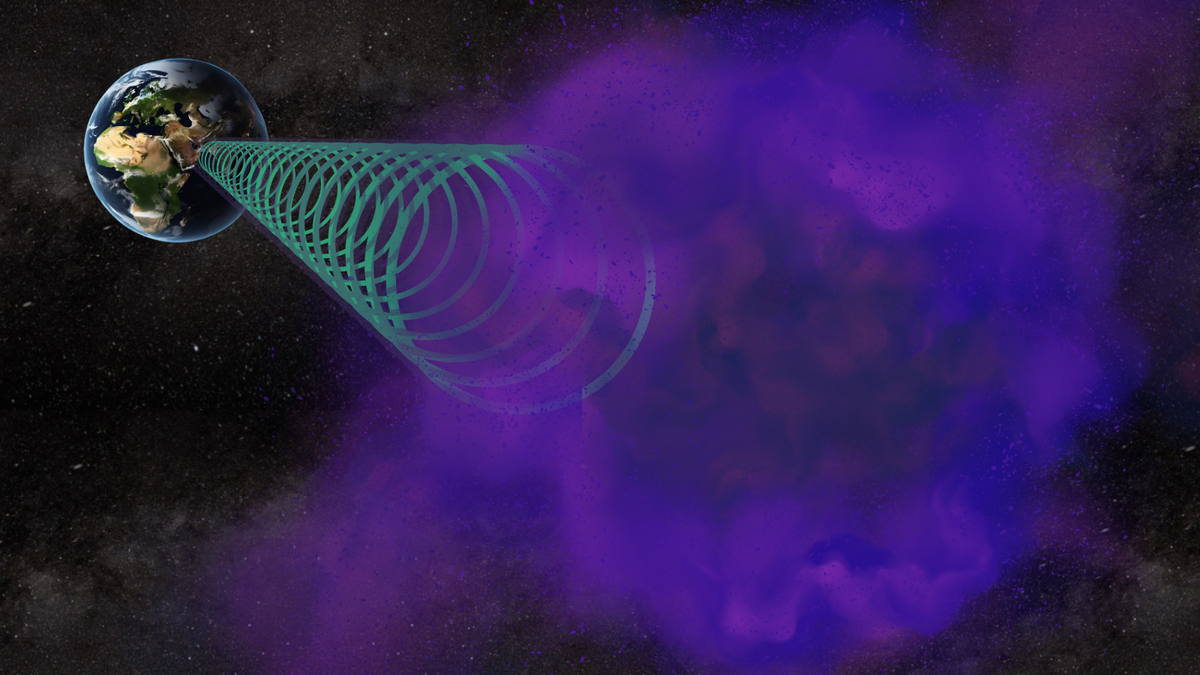
Researchers report a pathway that begins in the gut and ends with a potent pro-inflammatory toxin in brain cells contributing to the development of Alzheimer’s disease. (CREDIT: CC BY-SA 3.0)
Recent groundbreaking research spearheaded by Drs. Yuhai Zhao and Walter J Lukiw at the LSU Health New Orleans Neuroscience Center unveils a previously unknown pathway from the gut to the brain which may be a pivotal contributor to the onset of Alzheimer's disease (AD).
The fascinating twist? There’s also a relatively straightforward way to prevent this from happening. The study's results are now accessible in the esteemed scientific journal, Frontiers in Neurology.
At the heart of the discovery is a molecule teeming with a virulent microbial-generated neurotoxin. Named lipopolysaccharide (LPS) and sourced from the Gram-negative bacteria Bacteroides fragilis found in our gastrointestinal (GI) tract, the specific neurotoxin in question is identified as BF-LPS.
Dr. Lukiw expounds, “LPSs, in a broader sense, rank amongst the most potent microbial-derived pro-inflammatory neurotoxic glycolipids we know of.” He continues, “Various laboratories around the globe, ours included, have pinpointed diverse LPS variants within neurons in the brains affected by Alzheimer’s.”
To elucidate, the research meticulously maps out the journey of BF-LPS from the gut to the brain and its subsequent effects. The pathway is as follows: BF-LPS seeps out of the GI tract, bypasses the blood-brain barrier using the circulatory system, and then infiltrates various brain compartments.
Related Stories:
Its presence there induces inflammation within the brain cells and hinders the neurofilament light (NF-L) — a crucial protein that maintains cell stability. A depletion in NF-L can cause severe neuronal cell atrophy, resulting in eventual cell death, a phenomenon prominently seen in AD-affected neurons.
However, all is not lost. The research also uncovers a glimmer of hope — the entire process can be potentially thwarted with sufficient dietary fiber intake.
What sets this discovery apart are its three innovative aspects. Firstly, the AD-triggering pathway originates within our own bodies, specifically in our GI-tract microbiome, making it active and inherent throughout our existence. Secondly, the perilous neurotoxin, BF-LPS, is an organic outcome of our GI-tract's microbial metabolic processes. Lastly, controlling the abundance of Bacteroides fragilis in our microbiome, the neurotoxin's primary source, is achievable through our fiber intake.
Lukiw simplifies this: “From a dietary standpoint, balancing the microbial inhabitants of our microbiome can effectively regulate AD-related microbes and their potential to release neurotoxins like BF-LPS.”
This landmark study concludes with the assertion that enhanced comprehension of the intricate interplay between the GI tract-Central Nervous System axis, the GI-tract microbiome, and Alzheimer’s can pave the way for innovative diagnostic and therapeutic strategies in tackling AD and similar severe neurodegenerative disorders.
To provide context, current statistics indicate that Americans consume an average of 10-15 grams of fiber daily. However, the USDA recommends higher intakes; women below 50 should consume 25 grams, men 38 grams. Those over 50 should intake 21 and 30 grams respectively.
Alzheimer's remains a major health concern, being the predominant diagnosis for dementia patients and ranking sixth as a cause of death in the U.S. The National Institutes of Health estimates that about 5.8 million Americans aged 65 and older suffer from AD. Projections show that by 2050, this number could surge to 13.8 million.
This trailblazing research was a collaborative effort, with contributions from Drs. Vivian Jaber and Nathan Sharfman of LSU Health New Orleans and Aileen Pogue from Alchem Biotech Research in Toronto.
Funding was generously provided by LSU Health New Orleans, the Brown Foundation, the Joe and Dorothy Dorsett Innovation in Science Health Aging Award, and the National Institutes on Aging of the National Institutes of Health.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Joseph Shavit
Head Science News Writer | Communicating Innovation & Discovery
Based in Los Angeles, Joseph Shavit is an accomplished science journalist, head science news writer and co-founder at The Brighter Side of News, where he translates cutting-edge discoveries into compelling stories for a broad audience. With a strong background spanning science, business, product management, media leadership, and entrepreneurship, Joseph brings a unique perspective to science communication. His expertise allows him to uncover the intersection of technological advancements and market potential, shedding light on how groundbreaking research evolves into transformative products and industries.