Breakthrough wireless brain technology treats Parkinson’s without surgery
A new wireless nanoparticle therapy stimulates deep brain neurons and clears toxic protein buildup to restore function in Parkinson’s disease.
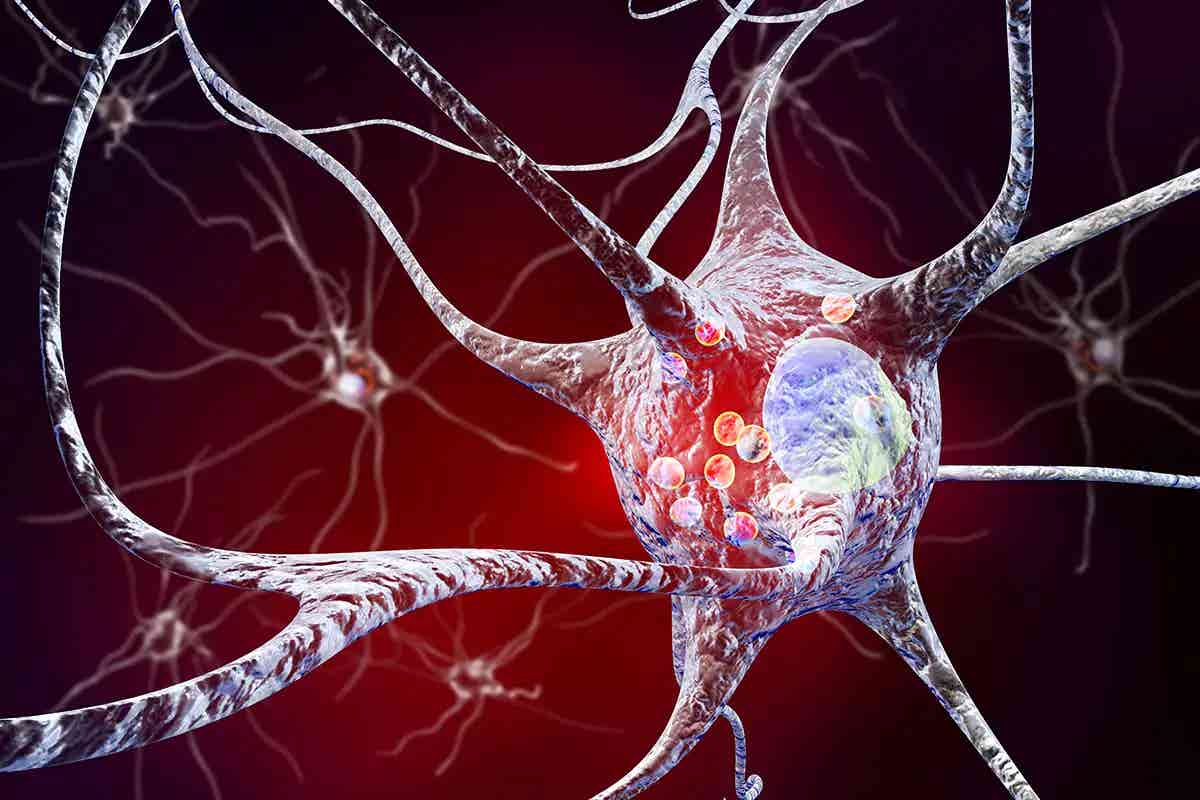
New wireless nanoparticles restore brain function in Parkinson’s mice using light, heat, and targeted cleanup of toxic proteins. (Science Photo Library)
Parkinson’s disease disrupts lives by slowly robbing people of their ability to move, speak, and function with ease. It's the second most common brain disorder that gets worse over time, and for many, its effects are devastating. The disease centers around a key problem in the brain—clumps of a protein called α-synuclein form harmful structures known as Lewy bodies.
These toxic bundles gather in a region of the brain called the substantia nigra, where they damage and kill dopamine-producing neurons. Without enough dopamine, the brain struggles to control movement, leading to tremors, stiffness, and slow movement.
Doctors have long relied on deep brain stimulation, or DBS, to help with symptoms. This involves implanting wires into the brain and sending electrical pulses to stimulate neurons. It can ease symptoms for many, but it also comes with risks.
Because it requires surgery, DBS can cause problems like memory loss, depression, or anxiety. In recent years, researchers have tested less invasive methods like transcranial magnetic stimulation, but those lack the precision and depth needed to reach key brain areas.
Now, a new breakthrough could change everything.
A Smarter, Safer Way to Stimulate the Brain
A group of scientists led by Prof. Chen Chunying from the National Center for Nanoscience and Technology has created a groundbreaking technology. Their work, published in Science Advances, introduces a wireless, non-invasive system that stimulates deep brain cells and clears harmful protein buildup without needing surgery.
This system, called ATB NPs, uses tiny gold-based particles designed to find, target, and treat damaged neurons deep in the brain. The name stands for its three parts: Au (gold nanoshells), TRPV1 (an antibody that finds special heat-sensitive receptors in neurons), and β-syn (a peptide that helps break down toxic α-synuclein).
Together, these nanoparticles act like tiny machines with a mission. They travel to a part of the brain hit hardest by Parkinson’s and go to work.
Related Stories
How These Nanoparticles Work
The brain contains neurons that have a special receptor called TRPV1. These receptors react to heat and help cells communicate. The new system uses this property to its advantage. Scientists inject the nanoparticles directly into the affected part of the brain using a method called stereotactic injection. The particles find and attach to dopamine-producing neurons thanks to their built-in antibody that recognizes TRPV1 receptors.
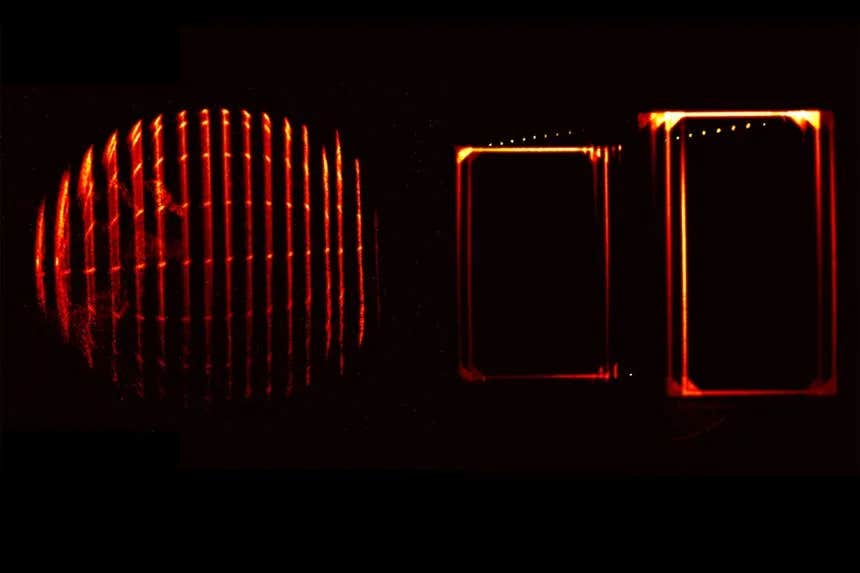
Once in place, the nanoparticles wait for a signal. That signal comes in the form of a pulsed near-infrared (NIR) laser aimed at the brain. This type of light can safely pass through the skull and deep into brain tissue. When the laser hits the gold nanoshells, they absorb the light and heat up.
This heat triggers the TRPV1 receptors, causing calcium ions to flood into the neuron. That influx sparks electrical activity, helping neurons fire again. But this system doesn’t just stimulate brain cells—it also helps clean them.
As the particles heat up and stimulate the neurons, they release β-syn peptides. These tiny molecules help break down α-synuclein by working with the brain’s natural cleanup system, known as chaperone-mediated autophagy. A protein called HSC70 kicks off this cleanup, helping cells clear out the toxic clumps that build up in Parkinson’s disease.
By combining stimulation and cleanup, the particles help restore the health of dopamine neurons and improve movement in affected mice.
Results That Could Redefine Treatment
In a lab setting, researchers tested the new system on mice with a Parkinson’s-like condition. These mice had been injected with α-synuclein fibrils, causing neuron damage in the same brain region that Parkinson’s affects in humans. After treatment with the nanoparticles and exposure to NIR light, the mice showed major improvement.
The treated mice moved better and more smoothly. Their brain cells released dopamine again. The buildup of harmful α-synuclein was greatly reduced. Most importantly, the damaged neuron network began to recover.
This shows that the ATB NPs not only restore function but also tackle the root of the disease. It’s a rare achievement in neuroscience: a system that can stimulate the brain without cutting it open, and heal it without altering its DNA.
Why This System Matters
This wireless deep brain stimulation system has three big advantages. First, it uses receptors already found in the brain. That means it doesn't need gene editing or permanent electrodes. Second, it offers very accurate control over when and where to stimulate. The near-infrared laser can be turned on and off at will and directed at precise brain areas. Third, the particles are safe. They break down naturally in the body and don’t cause harm.
This technology could also apply to other brain diseases where neurons degenerate, including Alzheimer’s or Huntington’s disease. Its flexibility and safety make it a strong candidate for future human trials.
As the lead researcher explained, "This system achieves precise modulation of degenerated neurons by directly stimulating the thermosensitive TRPV1 receptor in neurons.” That level of accuracy could open a new era in treating complex brain disorders.
While more testing remains before this technology can be used in hospitals, the science behind it is solid and full of promise. It represents a major leap forward in how scientists think about deep brain stimulation and neurodegenerative disease treatment.
Looking Ahead
If the wireless nanosystem succeeds in human trials, it could replace invasive brain surgery with a simple injection and light therapy. That would mean faster recovery, fewer side effects, and better outcomes for patients with Parkinson’s.
Instead of managing symptoms with risky surgery, doctors may soon help the brain heal itself—by using light, heat, and the power of nanotechnology. This discovery brings hope not just to those with Parkinson’s, but to millions of people worldwide who face the daily challenges of brain disorders.
Note: The article above provided above by The Brighter Side of News.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Mac Oliveau
Science & Technology Writer | AI and Robotics Reporter
Mac Oliveau is a Los Angeles–based science and technology journalist for The Brighter Side of News, an online publication focused on uplifting, transformative stories from around the globe. Passionate about spotlighting groundbreaking discoveries and innovations, Mac covers a broad spectrum of topics—from medical breakthroughs and artificial intelligence to green tech and archeology. With a talent for making complex science clear and compelling, they connect readers to the advancements shaping a brighter, more hopeful future.